[Plastische End-zu-End-Therapie der bulbären Urethrastriktur]
Amir Hamza 1Wolf Behrendt 1
Stefan Tietze 1
1 Klinik für Urologie und Andrologie, Klinikum St. Georg gGmbH, Leipzig, Germany
Zusammenfassung
Für bulbäre Harnröhrenstrikturen bis zu 2,5 cm in der Länge bleibt die einzeitige, plastische chirurgische Operation mit Exzision der Stenose und direkte End-zu-End-Anastomose das beste Verfahren, um eine hohe Erfolgsquote zu garantieren.
Dieser Rückblick zeigt die Ergebnisse von 21 Patienten, die bulbär End-zu-End-Anastomosen in der Zeit von 2010–2013 unterzogen wurden.
In 20 Fällen (95,3%) wurden gute Ergebnisse erzielt. Die Kriterien für den Erfolg wurden durch prä- und postoperative radiologische Diagnostik und Uroflowmetrie registriert.
Schlüsselwörter
Urethralstriktur, End-zu-End-Anastomose
Introduction
Urethral strictures are scarred constrictions of the urethra that lead to stranguria. The morphological correlative of the stricture is a scarred transformation of the urethra. With men their corpus spongiosum is included in the process of scarring. This is a reaction to the different stimuli and can lead to a complete replacement of the spongy scar tissue [1].
The prevalence of urethral strictures is estimated to be around 1% and is declining although the rate of endoscopical interventions is increasing, but it is combined with great suffering of the patient [2], [3].
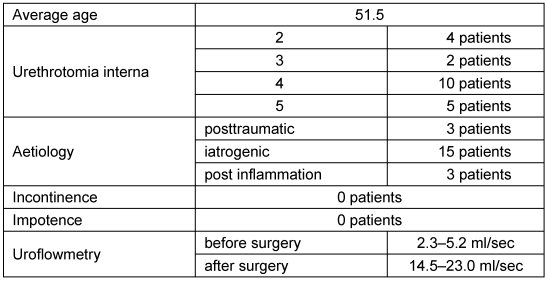
Urethral strictures result from varied causes. The biggest part is of iatrogenic origins, others are caused by traumas and infections. A rest of 30% remains unclear (see Table 1 [Tab. 1]) [1], [4].
Table 1: Causes of urethral strictures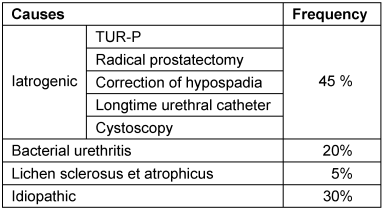
If urethral strictures are not discovered and treated in time, they can lead to a total damage of the urinary tract including permanent kidney failure.
Anatomy of the male urethra: The length of a male urethra of a grown-up person is about 20–25 cm and consists of 3 morphological and functional sections.
- Pars prostatica urethrae at the back extends from the Ostium urethrae internum to the colliculus seminalis.
- Pars membranace urethrae runs distally of the colliculus seminalis through the pelvic floor.
- Pars spongiosa urethrae (bulbar and penile parts of the urethra) extends from the pelvic floor to the meatus urethrae externus.
The diagnosis of the exact location and length of urethral strictures is the prior condition for a successful treatment. Therefore a good knowledge of the morphological and anatomical structures of the male urethra is important. The most frequent causes for bulbar strictures are idiopathic, followed by strictures after a transurethral resection. Altogether anterior strictures form more than 50% of all constrictions [5].
This paper only deals with bulbar urethral strictures with a length up to 2 cm, which were surgically treated with the technique of end-to-end anastomosis.
Material and method
21 patients who showed a bulbar stricture were operated in the time of February 1st, 2010 until July 30th, 2013. The average age of these patients was 51.5 years. The most frequent causes were of traumatic and iatrogenic nature. All patients had undergone 2 to 5 endoscopical operations (uretherotomia interna) before the plastical reconstruction of their urethra (see Table 2 [Tab. 2]). These patients complained about recurrent urinary infections resulting from residual urine. All patients underwent uroflowmetry before and after their surgery. Furthermore the stenoses were documented via retrograde urethrography. The clinical diagnostics were completed by sonography of the urinal tract, an assessment of continence and erection and duplex sonography of the exterior genital.
Urinary infections were antibiotically treated for 7 days before surgery.
Operation technique
The patient is laid in overextended lithotomy position to enable the access to the bulbar urethra (Figure 1 [Fig. 1]). The longitudinal section is the best possible incision and offers the best overview (Figure 2 [Fig. 2]). Having opened the Colles’ fascia the bulbar urethra is exposed (Figure 3 [Fig. 3]). The next step is the preparation of the fossa ischiorectalis by surgical sectioning of the M. transversus perinaei profundus. In the following the bulbus urethrae is mobilized and the bulbar urethra is laid open. The corpus spongiosum is exposed. After the detection and preparation of the stenosis two auxiliary sutures, one proximal and one distal of the stenosis, are placed in healthy urethra tissue. Then the urethra is longitudinally opened and explored. Afterwards the stenosis is resected and submitted for a histological screening. The proximal and distal ends of the urethra are cut in an angled method over a distance of 5 mm and tensionfree end-to-end re-anastomosed with 4x0 vicryl sewing material. A 18 Charr silicone catheter and a suprapubic catheter are placed. Now follows the layers’ wound closure combined with the insertion of a mini redon drainage which is removed the first day after surgery (Figure 4 [Fig. 4]). Prophylactic antibiosis is given for 3 days.
Figure 2: Longitudinal section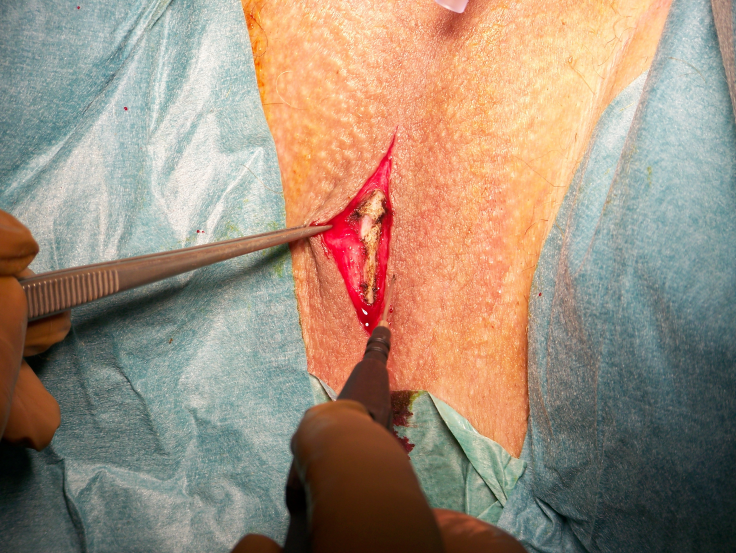
Figure 1: Positioning of the patient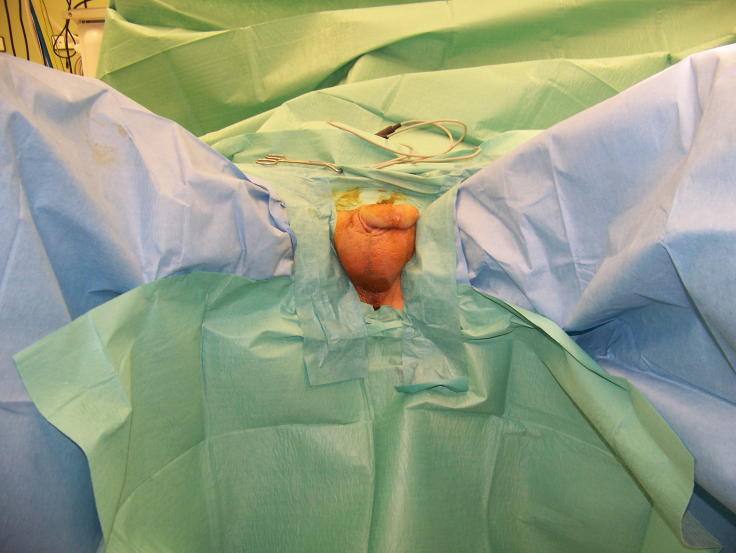
Figure 3: Preparation of the bulbar urethra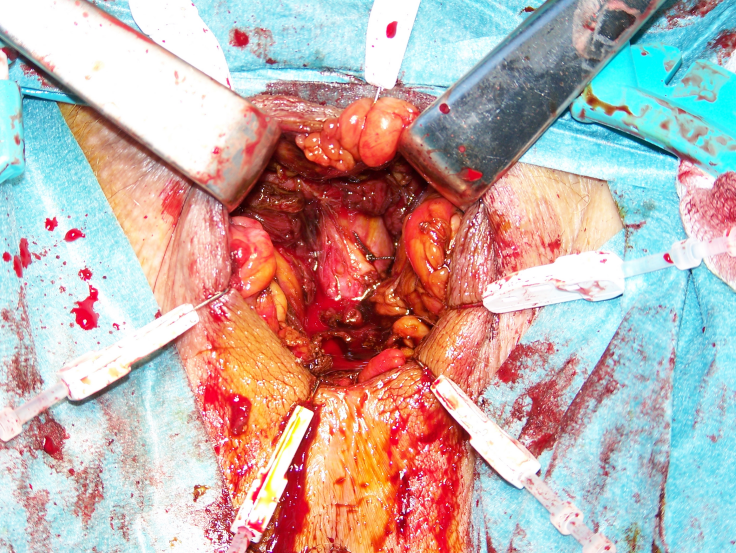
This catheter remains 14 days and is removed after an urethrography to document the anastomosis. Furthermore an uroflowmetry is done to mark of quality.
Results
The average duration of the operation was 70 min. One healing disorder complicated the normal postoperative course. The flow mesurement before the patients left hospital showed in 20 cases good micturition-value (14.5–23.0 ml/sec.) and the patients were satisfied. One patient showed no improvement of his micturition. No signs of incontinence or impotence as a consequence of the operation could be seen. The aftercare examinations took place two months after the surgery and showed satisfying results in 20 cases. The patient who showed no postoperative improvement had to undergo a frequent dilatation of his urethra. No reoperation was necessary in any patient.
Discussion
The resection of a short bulbar urethral stricture with end-to-end anastomosis offers a rate of success up to 90% [1], [4]. The diagnosis of the exact location and length of urethral strictures is the prior condition for a successful treatment. Therefore a complete uroradiological and endoscopical diagnosic must be done before surgery [6] (Figure 5 [Fig. 5]). The results of the end-to-end anastomosis concerning bulbar urinal strictures exceed by far the results of an exclusively endoscopical treatment (Urethrotomia interna) of strictures [6], [7] (Figure 6 [Fig. 6]). Our results confirm the findings of other work groups. The patients were satisfied with this method of operation. Therefore the indication for plastic surgical care of recurrent bulbar and membraneous urethral strictures must be set widely in order to avoid recurrent needless surgeries [1], [5], [6].
Figure 5: Preoperative urethrogram shows bulbar urethral stricture. 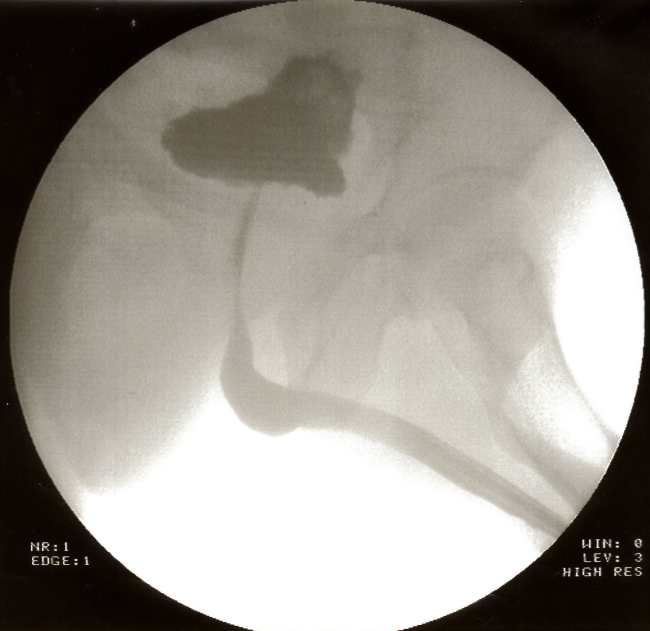
Figure 6: Urethrogram after direct end-to-end anastomosis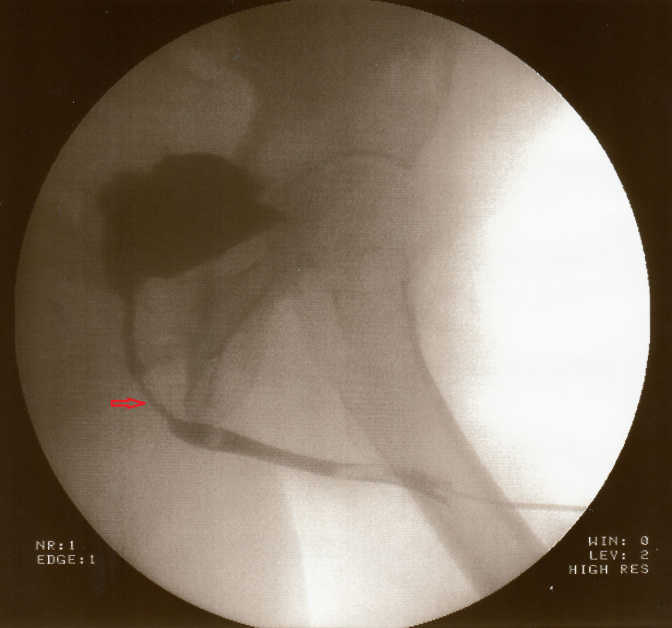
The described operation technique has improved within the last years and offers various possibilities without great morbidity [1], [6]. This operative approach helps to preserve the ability of erection by conservation of the vascular tissue of the penis and the Nn. cavernosi.
Our results match with results of other work groups.
Notes
Competing interests
The authors declare that they have no competing interests.
References
[1] Olianas R, Oberbeck D, Pottek T, Schreiter F. Bulbobulbäre und bulboprostatische Anastomose der Harnröhre [Bulbo-bulbar and bulbo-prostatic anastomosis of the urethra]. Urologe A. 1998 Jan;37(1):25-30. DOI: 10.1007/s001200050144[2] Barbagli G. Die perineale Urethrostomie bei komplexer vorderer Harnröhrenstriktur [Perineal urethrostomy in complex anterior urethral stricture]. Urologe A. 2010 Jun;49(6):731-3. DOI: 10.1007/s00120-010-2312-x
[3] Tritschler S, Roosen A, Füllhase C, Stief CG, Rübben H. Urethral stricture: etiology, investigation and treatments. Dtsch Arztebl Int. 2013 Mar;110(13):220-6. DOI: 10.3238/arztebl.2013.0220
[4] Hauser S, Fechner G, Ellinger J, Müller SC. Die plastische Rekonstruktion der Harnröhre [Urethral reconstructive surgery]. Urologe A. 2010 Jun;49(6):727-30. DOI: 10.1007/s00120-010-2311-y
[5] Lumen N, Hoebeke P, Willemsen P, De Troyer B, Pieters R, Oosterlinck W. Etiology of urethral stricture disease in the 21st century. J Urol. 2009 Sep;182(3):983-7. DOI: 10.1016/j.juro.2009.05.023
[6] Spahn M, Kocot A, Riedmiller H. Interventionelle und operative Behandlung der Harnröhrenenge: End-zu-End-Anastomose [Interventional and surgical treatment of urethral strictures. End-to-end anastomosis]. Urologe A. 2010 Jun;49(6):720, 722-6. DOI: 10.1007/s00120-010-2310-z
[7] Rödder K, Olianas R, Fisch M. Urethralstriktur – operative Konzepte [Urethral strictures – operative strategy]. Urologe A. 2006 Apr;45(4):499-511; quiz 512-3. DOI: 10.1007/s00120-006-1031-9