Increased mortality in hypernatremic burned patients
Thomas Namdar 1Frank Siemers 1
Peter L. Stollwerck 1
Felix H. Stang 1
Peter Mailänder 1
Thomas Lange 1
1 Department of Plastic and Hand Surgery, Burn Unit, University Hospital Schleswig-Holstein, Campus Lübeck, Germany
Abstract
Introduction: In-hospital hypernatremia develops usually iatrogenically from inadequate or inappropriate fluid prescription. In severely burned patient an extensive initial fluid resuscitation is necessary for burn shock survival. After recovering of cellular integrity the circulating volume has to be normalized. Hereby extensive water and electrolyte shifts can provoke hypernatremia.
Purpose: Is a hypernatremic state associated with increased mortality?
Method: Retrospective study for the incidence of hypernatremia and survival in 40 patients with a totally burned surface area (TBSA) >10%. Age, sex, TBSA, ABSI-Score and fluid resuscitation within the first 24 hours were analyzed. Patients were separated in two groups without (Group A) or with (Group B) hypernatremia.
Results: Hypernatremia occurred on day 5±1.4. No significant difference for age, sex, TBSA, ABSI-Score and fluid resuscitation within the first 24 hours were calculated. In Group A all patients survived, while 3 of the hypernatremic patient in Group B died during ICU-stay (Odds-ratio = 1.25; 95% CI 0.971–1.61; p=0.046).
Conclusion: Burned patients with an in-hospital acquired hypernatremia have an increased mortality risk. In case of a hypernatremic state early intervention is obligatory. There is a need of a fluid removal strategy in severely burned patient to avoid water imbalance.
Keywords
burn injury, hypernatremia, mortality, critical care
Introduction
The serum sodium level is closely controlled by water homeostasis, and mediated by thirst, vasopressin and renal function in healthy individuals [1]. Hypernatremia (serum sodium >146 mmol/l) is a common disorder [2]. In-hospital hypernatremia is frequently caused iatrogenically, resulting from inadequate or inappropriate fluid prescription in the setting of increased water loss [2], [3], [4]. Non-specific neurologic symptoms like light-headedness, nausea, headache, fatigue and confusion may be consistent in alert hypernatremic patients [5]. In unconscious patients, laboratory results have to be observed vigilantly, because of the lack of these unspecific symptoms [6].
Generally, in-hospital hypernatremia has a low incidence of 1–2% [4], [7], but appears to be associated with increased mortality rates range from 38% to 66% compared to normonatremic patients [4], [8], [9], [10], [11], [12], [13]. Hypernatremia appears more frequently in individuals with an altered status, unconscious patients, infants, and elderly patients (>65 years) [6], [8], [9] and is associated with the use of diuretics and co-morbidities – like renal insufficiency, diarrhea, or febrile illness [10], [14], [15]. In Intensive Care Units (ICUs) an acquired hypernatremic state is reported up to 7.9% [10], [11], [12], [13]. There is no data of survival of hypernatremic burned patients.
We present a retrospective study to elucidate in-hospital acquired hypernatremia and associated mortality.
Material and methods
40 patients with a totally burned surface area (TBSA) >10% were identified. Patients with a TBSA <10% were excluded from this study. All patients were treated during the first 24 hours after burn injury guided by the Parkland-Formula with 4 ml/kgT/BSA-% of Ringer's Lactate. No hypertonic infusate was infused. Hypernatremia was defined with serum sodium/creatinine levels ≥146 mmol/l. No patient presented elevated serum sodium levels on admission. In 15 patients a hypernatremic state was registered during ICU-stay. 25 patients without hypernatremia (serum sodium <145 mmol/l) were summarized.
In all patients arterial blood gas analysis was performed in a 1 to 3 hours interval for the analyzed period. Hypernatremia was treated immediately with an increased infusion rate of electrolyte free water (glucose 5%).
Statistics were performed with SPSS® 15.0 (SPSS Inc., Chicago, USA). To estimate significance Mann-Whitney-U- or CHI-square-test (for categorical variables) were performed. Results are written in mean value ± standard deviation.
Results
40 (12 female; 28 male) patients with a mean age of 47±19 years (minimum: 14 years; maximum: 83 years), a TBSA of 26±12% (minimum: 10%; maximum: 70%), and a mean ABSI-Score of 7.3±2 (minimum: 3; maximum: 11), were included. Mean partial thickness BSA was 20.7±11% and full thickness BSA was 5.1±6%. Twenty-four patients (60%) requiered mechanical venitilation. Patients were separated in two groups without (Group A) or with (Group B) hypernatremia.
In Group A 25 patients (7 female; 18 male) with a mean age of 47±18 years (minimum: 14 years; maximum: 73 years), a mean TBSA of 23±11% (minimum: 10%; maximum: 60%), and a mean ABSI-Score of 6.9±2.1 (minimum: 3; maximum: 11) were summarized. Mean partial thickness BSA was 19.4±8% and full thickness BSA was 3.8±5%. Ten patients requiered mechanical venitilation. No Total Parenteral Nutrition (TPN) was necessary in 3 individuals. Hypalbuminemia was registered in all 25 patients. Mean creatinine within the first 14 days after trauma was 72±17 µmol/l (minimum: 49 µmol/l; maximum: 105 µmol/l).
In Group B 15 patients (5 female; 10 male) with a mean age of 47±22 years (minimum: 17 years; maximum: 83 years), a mean TBSA of 30±13% (minimum: 12%; maximum: 70%), and a mean ABSI-Score of 8.1±1.7 (minimum: 5; maximum: 11) were included. Mean partial thickness BSA was 23.1±15% and full thickness BSA was 7.1±7%. Fourteen patients requiered mechanical venitilation. No Total Parenteral Nutrition (TPN) was necessary in one individual. Hypalbuminemia was registered in all 15 patients. Mean creatinine within the first 14 days after trauma was 89±20 µmol/l (minimum: 68 µmol/l; maximum: 147 µmol/l). Patients characteristics are displayed in Table 1 [Tab. 1].
Table 1: Patients characteristics (mean age (SD: standard deviation), sex, mean TBSA, mean ABSI, need of dialysis, parenteral nutrition, need of furosemid, count of hypalbuminemia) divided in Group A (without) and Group B (with hypernatremia)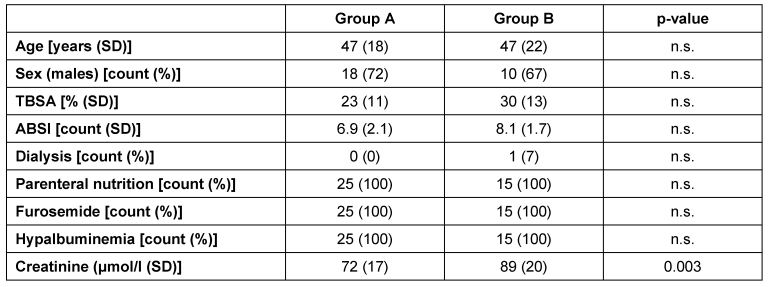
Hypernatremia occurred on day 5±1.4 after admission and persisted for 4.6±2.7 days.
3 patients (3 female) died during ICU-stay (34±8 days after trauma; range: 27 to 43 days). Mean age was 59±22 years (minimum: 41 years; maximum: 83 years), a mean TBSA of 26±6.6% (minimum: 20%; maximum: 33%) and mean ABSI-Score of 9.6±1.5 (minimum: 8; maximum: 11).
No significant difference for age, sex, TBSA, partial or full thickness BSA, ABSI-Score, TPN-count, diuretics and incidence of hypalbuminemia were calculated. There was neither a significant difference between Group A and B in fluid resuscitation amount within the first 24 hours (Group A vs. Group B [ml/kg/%-TBSA]: 4.9±3 vs. 5.8±3; p=0.32), nor in daily IDR for day 3 to day 14 (Group A vs. Group B [ml]: 932±332 vs. 1,134±548; p=0.1), nor in IDR-TBSA-ratio for day 3 to day 14 (Group A vs. Group B [ml/%]: 6.6±10 vs. 3±2; p=0.113) (Table 2 [Tab. 2]).
Table 2: Mean daily infusion-diuresis-ratio (SD: standard deviation) in relation to body-weight and/or TBSA for the first 24 hours, day 3 to day 14, day 3 to day 6 after burn injury and ICU mortality and in-hospital mortality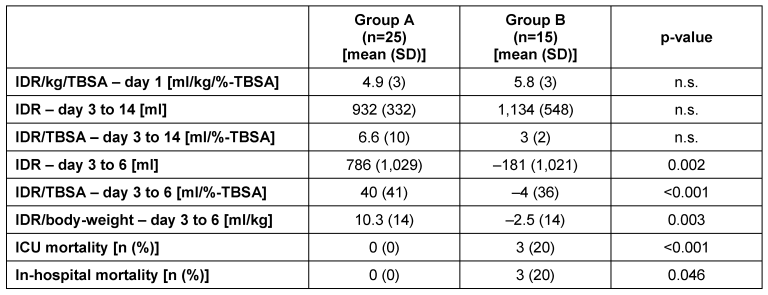
Statistical analysis of the period from day 3 to 6 showed a significant higher daily IDR-amount in Group A (Group A vs. Group B [ml]: 786±1,029 vs. –181±1,021; p=0.002) and daily IDR-TBSA-ratio (Group A vs. Group B [ml/%]: 40±41 vs. –4±36; p<0.001). There was also a significant higher daily infused volume per kilogram body-weight for the period from day 3 to day 6 (Group A vs. Group B [ml/kg]: 10.3±14 vs. –2.5±14; p=0.003.
A significant association of mechanical ventilation and the incidence of hypernatremia was found (ODDS-ratio: 21 (95% Confidence Intervall: 2.4–186, p=0.001).
In Group A all patients survived and 3 (20%) of the hypernatremic patient died (Odds-ratio: 1.25; 95% Confidence Interval: 0.971–1.61; p=0.046) during ICU-stay. 2 patients died in a septic state due to pneumonia, and 1 patient died in a multi organ failure. Within Group B there was no significant difference between hypernatremic survivors and non-survivors in mean age, sex, TBSA, ABSI, TPN-count, diuretics, incidence of hypalbuminemia, initial burn shock resuscitation, IDR/TBSA-ratio (day 3 to 6) and IDR/TBSA-ratio (day 3 to 14).
Discussion
Systemic effects of burn injury are not limited to the injured area. In severely burned patients microvascular integrity is lost and a plasma-like fluid leaks into the interstitial space. Therefore extensive fluid resuscitation becomes obligatory to ensure oxygen delivery [16]. The time after injury at which capillary integrity is restored differs individually [17]. After burn shock resuscitation and recovery of cellular integrity circulating fluid volume has to be normalized. The fluid removal has to be done carefully to avoid systemic dehydration, which causes cell death and leads to an increase in the depth of necrotic tissue [18]. Hereby extensive water and electrolyte shifts are provoked. Even a short period of systemic dehydration (respectively hypernatremia) may lead to an induction of apoptosis and burn wound deepening apart of its neurologic effects [19], [20].
Despite years of experience several variations exist in resuscitation practices around the world. The Parkland formula – which uses Ringer's Lactate – is the most frequently used formula [21]. On the other hand hypernatremic solutions have been known for many years in burn shock treatment [22], [23]. The hypernatremic serum is supposed to decrease tissue edema, escharotomies and endotracheal intubation. But there is no consensus regarding the type of osmolarity of hypertonic resuscitation fluid [24]. At least, there is no evidence of increased mortality after burn injury in patients treated with hypernatremic solutions.
There are three fundamental principles of water and sodium cellular physiology [5].
- To maintain osmotic equilibrium water freely shifts between intra- and extracellular space, allowing osmolality. Sodium – the predominant effective extracellular solute – and its serum concentration closely reflects plasma osmolality.
- A normal kidney will attempt to reabsorb or excrete solute-free water to preserve a normal plasma osmolality of 275 to 290 mOsm/kg. Arginine vasopressin is the primary hormone regulating plasma osmolality [25]. Vasopressin release is modulated by osmoreceptors [26], [27] and functions at the distal collecting kidney duct to increase water reabsorption [28]. In conscious patients wide fluctuations in water and sodium intake, can maintain serum osmolality in a narrow range (275 to 290 mOsm/kg) [29].
Hypotension and hypovolemia also trigger vasopressin release. Other triggers for vasopressin release include pain, nausea, thirst and acidosis [30], [31]. - Rapid transcellular water shifts can lead to cellular damage. In a normal steady-state environment, free water diffuses in and out of the intracellular space to maintain osmotic equilibrium. Significant fluid shifts associated with serum sodium disorders, and major cellular volume changes can lead to cell damage and cell death [5]. As an initial compensatory mechanism to preserve cellular volume, there is a rapid shift of sodium, potassium, chloride and water either out (hyponatremia) or into cells (hypernatremia). After 48 to 72 hours, a slower adaptive phase takes effect and organic osmolytes are mobilized additionally to maintain normal cellular volume.
Hypernatremia is easy to evaluate (i.e. blood gas analysis) in an ICU setting [32]. The patients' free water deficit can be calculated by using the formula of Adrogué et al. [33] – calculating the effect of 1 liter of any infusate on serum sodium concentration (Figure 1 [Fig. 1]). A replacement strategy using a correction rate of 12 mmol/l serum sodium per day should be utilized to avoid cerebral edema [32]. On the other hand, in-hospital hypernatremia is a common electrolyte disorder – frequently caused iatrogenically – and is a valid sign for systemic dehydration [3], [5], [34]. Aiyagari et al. [10] identified osmotic agents as the most frequent cause of in-hospital hypernatremia.
Figure 1: The formula of Adrogué et al. (33) offers an easy way to estimate the effect of 1 liter of any infusate on change in serum sodium concentration. Total body water is calculated as a fraction of body weight (children: 0.6; non-elderly women: 0.5; elderly women: 0.45; non-elderly men: 0.6; elderly men: 0.5).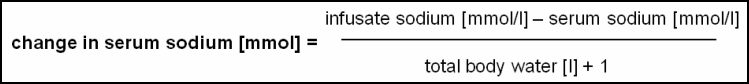
In our study, a hypernatremic state was registered in 37.5% of patients with a TBSA >10%. This data is comparable to previous studies in critically ill patients [4], [10], [11], [12], [35]. Mackie et al. [36] reported that mechanical ventilation leads to an increased fluid loss in burned patients. We also found a significant association of hypernatremia and mechanical ventilation. This supports the findings of Mackie et al. [36].
The mortality rate in our study was lower than in other studies (38% to 66%) [4], [8], [9], [10], [11], [12], [13] (Table 3 [Tab. 3]). This may be contributed to the larger populations analyzed in these studies, but they present a mix of medical, surgical, neurosurgical and neurological patients and did not separate a burn injury subgroup. O'Donoghue et al. [35] found an incidence of hypernatremia in 7.7% of 3,317 patients in a mixed medical/general surgery ICU. Polderman et al. [13] studied 389 patients on a medical ICU of which 5.7% developed hypernatremia. Lindner et al. [12] studied 981 patients in a medical ICU and reported an incidence of in-hospital hypernatremia of 7.0%. Aiyagari et al. [10] studied 4,296 patients admitted to a neurosurgical ICU and found 7.9% hypernatremic patients. Hoorn et al. [11] found an incidence of 7.1% for acquired hypernatremia in a mixed general, surgical and neurological ICU population. Mandal et al. [9] found a mortality rate of 66% in a mixed patients collective (n=116). O'Connor et al. [8] found hypernatremia in 2.1% of 336 elderly patients (mean age 81.4 years) in a cross-sectional study. Palevsky et al. [4] found a mortality rate of 41% in 116 hypernatremic patients admitted to a 942-bed urban medical-surgical hospital.
Table 3: Summary of recent studies focused on the survival of patients with in-hospital acquired hypernatremia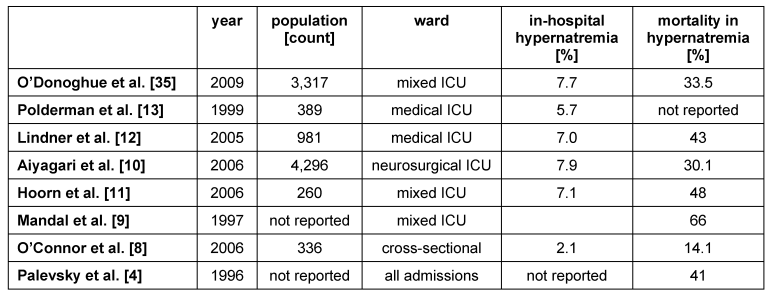
Thus, severely burned patients have an increased risk of systemic fluid imbalance. We assume that a hypernatremic state after burn injury results from extensive fluid resuscitation/removal therapy. The extensive infused amounts of saline infusion during initial burn shock therapy and the transdermal fluid loss in partially injured surface areas, complicate a well equilibrated intravasal fluid volume.
The reason why there was an increased mortality in the hypernatremic patients remains unclear and could not be identified in our study. For this purpose the analyzed population was not numerous enough. One explanation for the increased mortality in hypernatremic burned patients might be that higher doses of infused/removed volume – even if no significance could be shown – were required. Therefore more extensive electrolyte disorders were induced. But we cannot maintain this assumption, because of the small size of the hypernatremic subgroup analyzed in our study.
Even the previously reported studies, focused on hypernatremia and mortality, could not elaborate the specific mechanisms by which hypernatremia leads to increased mortality [4], [8], [9], [10], [11], [12], [13], [35].
Limitations
In this retrospective study we analyzed only a small population of hypernatremic patients. There was no standardized protocol for fluid removal after burn shock. Therefore the incidence of a hypernatremic state in severely burned patients is not representative in this study. There was at least no standardized protocol for fluid therapy in hypernatremic patients. The collected values and findings only have an empiric character and should be investigated by prospective randomized clinical trials.
Conclusions
Our findings support the prior reported systemic effects of water imbalance. Even in specialized burn units incidence of hypernatremia is unavoidable. A lot of attention is paid to the initial fluid resuscitation in severely burned patients and so there are several well established algorithms of burn shock therapy during capillary hyperpermeability [12], [13], [17]. There is still a lack of researched algorithms of fluid removal after burn shock treatment. In case of systemic dehydration (respectively hypernatremia), because of its consequences early intervention is obligatory. Blood gas analysis should be performed routinely in short intervals. Patients with an in-hospital acquired hypernatremia have an increased mortality risk. There is a need of an established fluid removal strategy in severely burned patients to avoid water imbalance.
Notes
Conflicts of interest
None declared.
References
[1] Gennari FJ. Current concepts: Serum osmolality: Uses and limitations. N Engl J Med. 1984;310(2):102-5.[2] Adrogue HJ, Madias NE. Hypernatremia. N Engl J Med. 2000;342(20):1493-9. DOI: 10.1056/NEJM200005183422006
[3] Snyder NA, Feigal DW, Arieff AI. Hypernatremia in elderly patients: A heterogeneous, morbid, and iatrogenic entity. Ann Intern Med. 1987;107(3):309-19.
[4] Palevsky PM, Bhagrath R, Greenberg A. Hypernatremia in hospitalized patients. Ann Intern Med.1996;124(2):197-203.
[5] Lin M, Liu SJ, Lim IT. Disorders of water imbalance. Emerg Med Clin North Am. 2005;23(3):749-70, ix. DOI: 10.1016/j.emc.2005.03.001
[6] Gennari FJ. Hypo-hypernatremia: disorders of water imbalance. In: Davison AM, editor. Oxford textbook of clinical nephrology. Oxford: Oxford University Press; 1998. p. 175-200.
[7] Long CA, Marin P, Bayer AJ, Shetty HG, Pathy MS. Hypernatraemia in an adult in-patient population. Postgrad Med J. 1991;67(789):643-5. DOI: 10.1136/pgmj.67.789.643
[8] O'Connor KA, Cotter PE, Kingston M, Twomey C, O'Mahony D. The pattern of plasma sodium abnormalities in an acute elderly care ward: a cross-sectional study. Ir J Med Sci. 2006;175(3):28-31.
[9] Mandal AK, Saklayen MG, Hillman NM, Markert RJ. Predictive factors for high mortality in hypernatremic patients. Am J Emerg Med. 1997;15(2):130-2. DOI: 10.1016/S0735-6757(97)90082-6
[10] Aiyagari V, Deibert E, Diringer MN. Hypernatremia in the neurologic intensive care unit: how high is too high? J Crit Care. 2006;21(2):163-72. DOI: 10.1016/j.jcrc.2005.10.002
[11] Hoorn EJ, Betjes MG, Weigel J, Zietse R. Hypernatraemia in critically ill patients: too little water and too much salt. Nephrol Dial Transplant. 2008;23(5):1562-8. DOI: 10.1093/ndt/gfm831
[12] Lindner G, Funk GC, Schwarz C, Kneidinger N, Kaider A, Schneeweiss B, Kramer L, Druml W. Hypernatremia in the critically ill is an independent risk factor for mortality. Am J Kidney Dis. 2007;50(6):952-7. DOI: 10.1053/j.ajkd.2007.08.016
[13] Polderman KH, Schreuder WO, Strack van Schijndel RJ, Thijs LG. Hypernatremia in the intensive care unit: an indicator of quality of care? Crit Care Med. 1999;27(6):1105-8. DOI: 10.1097/00003246-199906000-00029
[14] Phillips PA, Bretherton M, Johnston CI, Gray L. Reduced osmotic thirst in healthy elderly men. Am J Physiol. 1991;261(1 Pt 2):R166-71.
[15] Bruck E, Abal G, Aceto T Jr. Pathogenesis and pathophysiology of hypertonic dehydration with diarrhea: A clinical study of 59 infants with observations of respiratory and renal water metabolism. Am J Dis Child. 1968;115(2):122-44.
[16] Baxter CR, Shires T. Physiological response to crystalloid resuscitation of severe burns. Ann N Y Acad Sci. 1968;150(3):874-94. DOI: 10.1111/j.1749-6632.1968.tb14738.x
[17] Pham TN, Cancio LC, Gibran NS. American Burn Association practice guidelines burn shock resuscitation. J Burn Care Res. 2008;29(1):257-66.
[18] Heimbach D, Engrav L, Grube B, Marvin J. Burn depth: a review. World J Surg. 1992;16(1):10-5. DOI: 10.1007/BF02067108
[19] Harada T, Izaki S, Tsutsumi H, Kobayashi M, Kitamura K. Apoptosis of hair follicle cells in the second-degree burn wound unders hypernatremic conditions. Burns. 1998;24(5):464-9. DOI: 10.1016/S0305-4179(98)00034-5
[20] Kuroda T, Harada T, Tsutsumi H, Kobayashi M. Hypernatremia deepens the demarcating borderline of leukocytic infiltration in the burn wound. Burns. 1997;23(5):432-7. DOI: 10.1016/S0305-4179(97)00016-8
[21] Greenhalgh DG. Burn resuscitation: the results of the ISBI/ABA survey. Burns. 2010;36(2):176-82. DOI: 10.1016/j.burns.2009.09.004
[22] Monafo WW, Chuntrasakul C, Ayvazian VH. Hypertonic sodium solutions in the treatment of burn shock. Am J Surg. 1973;126(6):778-83. DOI: 10.1016/S0002-9610(73)80070-4
[23] Monafo WW, Halverson JD, Schechtman K. The role of concentrated sodium solutions in the resuscitation of patients with severe burns. Surgery. 1984;95(2):129-35.
[24] Herndon T. Total burn care. 3rd ed. Philladelphia: Saunders; 2007.
[25] Abramow M, Beauwens R, Cogan E. Cellular events in vasopressin action. Kidney Int Suppl. 1987;21:S56-66.
[26] Dunn FL, Brennan TJ, Nelson AE, Robertson GL. The role of blood osmolality and volume in regulating vasopressin secretion in the rat. J Clin Invest. 1973;52(12):3212-9. DOI: 10.1172/JCI107521
[27] McKinley MJ, Mathai ML, McAllen RM, McClear RC, Miselis RR, Pennington GL, Vivas L, Wade JD, Oldfield BJ. Vasopressin secretion: osmotic and hormonal regulation by the lamina terminalis. J Neuroendocrinol. 2004;16(4):340-7. DOI: 10.1111/j.0953-8194.2004.01184.x
[28] Berliner RW, Levinsky NG, Davidson DG, Eden M. Dilution and concentration of the urine and the action of antidiuretic hormone. Am J Med. 1958;24(5):730-44. DOI: 10.1016/0002-9343(58)90377-2
[29] Zerbe RL, Henry DP, Robertson GL. Vasopressin response to orthostatic hypotension. Etiologic and clinical implications. Am J Med. 1983;74(2):265-71. DOI: 10.1016/0002-9343(83)90625-3
[30] Robertson GL. Antidiuretic hormone: Normal and disordered function. Endocrinol Metab Clin North Am. 2001;30(3):671-94, vii. DOI: 10.1016/S0889-8529(05)70207-3
[31] Wood CE, Chen HG. Acidemia stimulates ACTH, vasopressin, and heart rate responses in fetal sheep. Am J Physiol. 1989;257(2 Pt 2):R344-9.
[32] Sterns RH. Hypernatremia in the intensive care unit: instant quality – just add water. Crit Care Med. 1999;27(6):1041-2. DOI: 10.1097/00003246-199906000-00005
[33] Adrogue HJ, Madias NE. Aiding fluid prescription for the dysnatremias. Intensive Care Med. 1997;23(3):309-16. DOI: 10.1007/s001340050333
[34] Janz T. Sodium. Emerg Med Clin North Am. 1986;4(1):115-30.
[35] O'Donoghue SD, Dulhunty JM, Bandeshe HK, Senthuran S, Gowardman JR. Acquired hypernatraemia is an independent predictor of mortality in critically ill patients. Anaesthesia. 2009;64(5):514-20. DOI: 10.1111/j.1365-2044.2008.05857.x
[36] Mackie DP, Spoelder EJ, Paauw RJ, Knape P, Boer C. Mechanical ventilation and fluid retention in burn patients. J Trauma. 2009;67(6):1233-8; discussion 1238. DOI: 10.1097/TA.0b013e3181be9c67




