[Silbernanopartikel als aktiver Bestandteil nicht-alkoholhältiger Mundspüllösungen]
Marzieh Fattahi-Dolatabadi 1Sedigheh Mehrabian 1
Babak Asghari 2
Amirmorteza Ebrahimzadeh Namvar 2
Fatemeh Ezzatifar 2
Abdolaziz Rastegar Lari 2
1 Department of Microbiology, Faculty of Biology Sciences, Branch of North Tehran, Islamic Azad University, Tehran, Iran
2 Antimicrobial Resistance Research Center and Department of Microbiology, Faculty of Medicine, Iran University of Medical Sciences, Tehran, Iran
Zusammenfassung
Zur Prävention von Mundhöhleninfektionen bei Immunsupprimierten und Krebspatienten wurde ein nicht irritierendes Alkohol-freies antiseptisch wirksames Mundspülmittel auf Basis geringer Mengen an Silbernanopartikeln (SNP) entwickelt.
Geprüft wurde die MIC und die MBC (MFC) von SNP im Konzentrationsbereich von 50–0,024 µg/ml mit und ohne Zusatz von 3% Ethanol (30.000 µg/ml) gegenüber S. mutans, S. aureus, E. coli, P. aeruginosa und C. albicans.
Die MIC betrug 0,78–3,12 µg/ml, die MBC 1,56–12,5 µg/ml, wobei alle Mikroorganismen erfasst wurden. Die Wirksamkeit unterschied sich nicht zwischen dem Ethanol-haltigen und dem Ethanol-freien Mundspülmittel. Da Ethanol speziell auf die empfindliche oder entzündete Schleimhaut irritierend wirkt, kann SNP als geeignete Alternative für 3% Ethanol angesehen werden.
Schlüsselwörter
Silbernanopartikel, Ethanol-freies Mundspülmittel, Immunsupprimierter
1 Background
In immunocompromised patients, the oral cavity is a common colonization site for a number of multidrug resistant bacterial and fungal microorganisms that can cause infections. In immunocompromised patients the oral candidiasis is highly widespread [1]. Over the past few decades an increase has been shown in the number of immunocompromised patients, partly caused by the rise in the numbers of bone marrow and solid organ transplantation, the increasing number of patients needs critical care, and the aggressive use of chemotherapy and radiation therapy [3]. In addition, Candida-associated stomatitis is also a recognized complication in elderly denture users, especially when denture hygiene is lacking [37]. Epstein and colleagues found out that oropharyngeal colonization by Candida species was common in recipients of hematopoietic cell transplants, despite systemic and topical antifungal prophylaxis [15]. The rate of fungal microorganisms such as Candida species causing nosocomial bloodstream infections in the USA or UK are high. Although Candida species are part of the normal mouth flora in 25–50% of healthy individuals, often called as asymptomatic colonization [27] where Candida are more prone to cause symptomatic disease than asymptomatic colonization. Within five years of seroconversion, up to 26% of HIV positive patients developed oral candidiasis, which is seen also in 12–100% of cancer patients undergoing chemotherapy, according to a published analysis of 15 studies, in 76% of patients undergoing bone marrow transplant and in up to 77% of carefully followed-up asthmatics using inhaled corticosteroids [41]. Silver and its derivatives is the oldest antimicrobial agent in traditional medicine [19]. Compounds containing Ag are not suitable as a cosmetic preservative because they gradually precipitate in sanitizing products and cosmetics. This precipitation reduces antimicrobial effects of silver. Ag nanoparticles are stable in solutions and their antimicrobial properties can remain for a long tie and therefore can be used as a preservative in sanitizing products and cosmetics [22]. SNP release silver ions with positive charge. These ions may cling to DNA and proteins, because these molecules contain compounds with negative charge, such as phosphorus and sulfur. Futhermore, Ag ions may cling to the surface of the microorganisms cause disruption in the integrity of cell wall [38]. In this study, concentrations of the SNP are lower than of ethanol.
The aim of the study was to develop an efficacious antimicrobial alcohol-free mouthwash containing SNP that is non-irritant, and would be useful for the oral care of immunocompromised patients, such as patients with cancer, HIV patients, and etc. We tested the solution against Candida albicans, a common cause of fungal infections in cancer patients, as well as against Pseudomonas aeruginosa, and Staphylococcus aureus, all being common sources of infection in immunocompromised patients. In addition, we used this solution against Streptococcus mutans that causes dental caries.
2 Materials and methods
2.1 SNP
Colloidal solution of SNP was obtained from the Nano Nasb Pars Co. (Tehran, Iran). Concentration of SNP was 4,000 µg/ml. Transmission electron microscopic (TEM) was used to determine the shape and size of the SNP.
2.2 Preparation of microorganisms
In this study, Escherichia coli ATCC 8739, Pseudomonas aeruginosa ATCC 9027 was used as Gram-negative bacteria, Staphylococcus aureus ATCC 6538, Streptococcus mutans 25175 as Gram-positive bacteria and Candida albicans ATCC 190231 as yeast. Bacterial strains were inoculated on the surface of TSA medium and Candida albicans was inoculated on sabouraud dextrose agar (SDA) medium then these mediums were incubated at 37°C (centigrade) for 24 hours. Solution of NaCl (0.9%) was used for preparation of microbial suspensions. During this suspension, last density of microorganisms was 108 CFU/mL. It was used as inoculums [28]. Inoculums density for each strain was confirmed by enumeration of bacteria by serial dilution and colony count also optical density (OD) of microbial suspension was adjusted by spectrophotometer to 0.1 at 600 nm.
2.3 Preparation of the mouthwash solution
In this study, mouthwash was obtained from the Tolid Daru Co. (Tehran, Iran). We prepared a mouthwash without alcohol. It was prepared from 0.6% of propylene glycol, 0.2% of fluoride sodium, 0.03% of mint essence, and 0.0004% of saccharin sodium. We used this mouthwash as a control (In order to compare antimicrobial effect of ethanol with SNP, we removed 0.1% of benzoat sodium from instruction.). Instructions and materials for preparing this mouthwash were obtained from Tolid Daru Co. too. Concentration of ethanol in the original mouthwash was 30,000 µg/ml (3%) and we compared this concentration of ethanol with SNP.
2.4 Measurement of minimum inhibitory and bactericidal (fungicidal) concentration (MIC and MBC, MFC)
MIC and MBC (MFC for yeast) were determined by a tube broth macrodilution method accordingly, 13 tubes containing 1 ml of broth medium with serial dilutions of SNP (in the concentration range of 50–0.19 µg/ml) were inoculated with test strains (final cell density of 106 CFU/mL) and incubated at 37°C for 24 hours. The lowest concentration of silver nanoperticles (SNP), showing growth inhibition (as seen visually) was considered as the minimum inhibitory concentration. The minimum bactericidal (fungicidal) concentration was recorded as the lowest concentration of the SNP that showed no growth on agar plates after spot inoculation and incubation for 24 hours. The assay was performed with proper controls (uninoculated medium and medium without SNP) [38]. In this study, concentration of ethanol in original mouthwash (30,000 µg/ml) was used.
2.5 Study of antimicrobial properties of SNP and ethanol
Challenge test [12], [13] was used to compare antimicrobial effects of SNP and ethanol. In this method, we provided three different samples of mouthwash such as mouthwash without antimicrobial agents and mouthwash containing one of the treatments (SNP at MIC and two lower concentrations or ethanol of 30,000 µg/ml) for each tested microorganisms. 1 ml of microbial suspension containing 108 CFU microorganism was inoculated with 100 ml of each sample then, 1 ml of each sample was removed at specified intervals of time (0, 2, 5 and 10 minutes) and was transferred to the TSA plate after a proper dilution (dilution is necessary in order to remove remaining SNP). These plates were incubated at 37°C for 24 hours. The consideration was performed in two issues. Finally the number of colonies on the plates was counted.
3 Results
3.1 Characterization of SNP
Shape and size of the SNP were determined by transmission electron microscopy. The TEM image has been illustrated in Figure 1 [Fig. 1]. This figure shows the size of SNP rang 10–40 nm, they are also spherical.
Figure 1: Micrograph of silver nanoparticles in transmission electron microscope
3.2 Minimum inhibitory and bactericidal (fungicidal) concentration
MIC and MBC (MFC) values of SNP toward microorganisms are summarized in Table 1 [Tab. 1]. It is clear from Table 1 [Tab. 1] that SNP has shown high antimicrobial activity toward all of the used microorganisms. MIC and MBC values of SNP toward two Gram-positive bacteria (S. mutans and S. aureus) were different. The most susceptible and resistant microorganisms were C. albicans and S. aureus.
Table 1: MIC and MBC (µg/ml) values of SNP†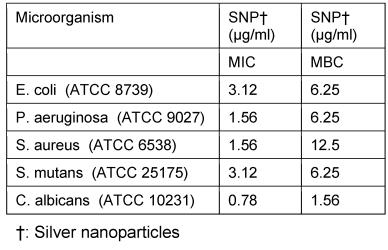
3.3 Study of preservative properties of SNP and ethanol
The results revealed that mouthwash containing SNP at MIC and two lower concentrations was completely effective within 0–5 minute but the mouthwash which contained SNP of 0.4 µg/ml killed S. aureus completely during 10 minutes. In this study antimicrobial effects of the ethanol-free mouthwash containing SNP (different concentrations) and mouthwash containing two treatments (SNP with different concentrations and ethanol of 30,000 µg/ml) against all of the microorganisms were identical (data no showed). SNP (different concentrations) killed all of the microorganisms faster than ethanol. Results of antimicrobial effects of SNP (different concentrations) and ethanol (30,000 µg/ml) at intervals of time (0–10 minutes), are represented in Table 2 [Tab. 2], Table 3 [Tab. 3], Table 4 [Tab. 4], Table 5 [Tab. 5], Table 6 [Tab. 6].
Table 2: Comparison of antimicrobial potency of SNP† (MIC and two lower concentrations) and Ethanol (30,000 µg/ml) at intervals of time (0–10 minutes) for E. coli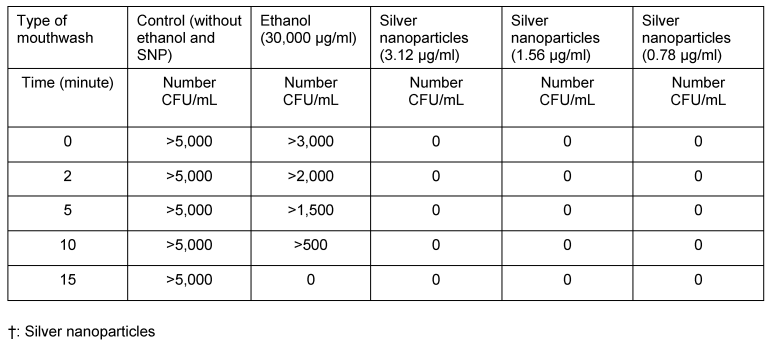
Table 3: Ability of SNP† (MIC and two lower concentrations) and ethanol (30,000 µg/ml) at intervals of time (0–10 minutes) for P. aeruginosa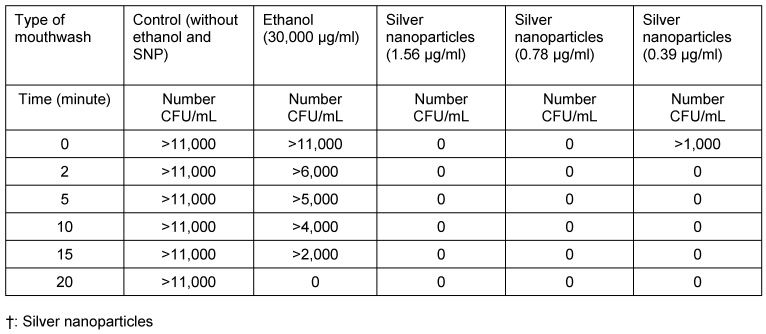
Table 4: Comparison of antimicrobial potency of SNP† (MIC and two lower concentrations) and ethanol (30,000 µg/ml) at intervals of time (0–10 minutes) for S. aureus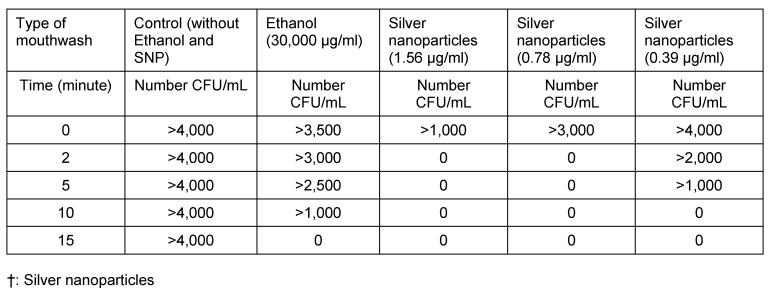
Table 5: Comparison of antimicrobial potency of SNP† (MIC and two lower concentrations) and ethanol (30,000 µg/ml) at intervals of time (0-10 minutes) for S. mutans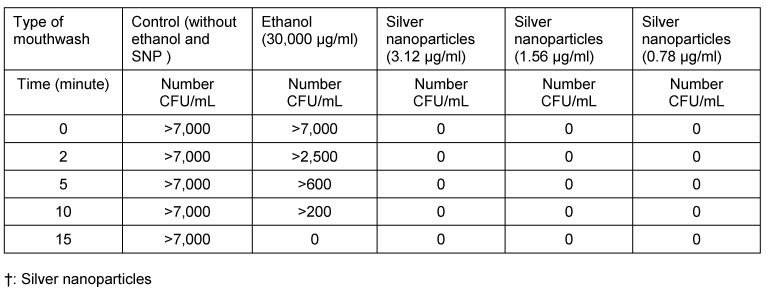
Table 6: Comparison of antimicrobial potency of SNP† (MIC and two lower concentrations) and Ethanol (30,000 µg/ml) at intervals of time (0–10 minutes) for C. albicans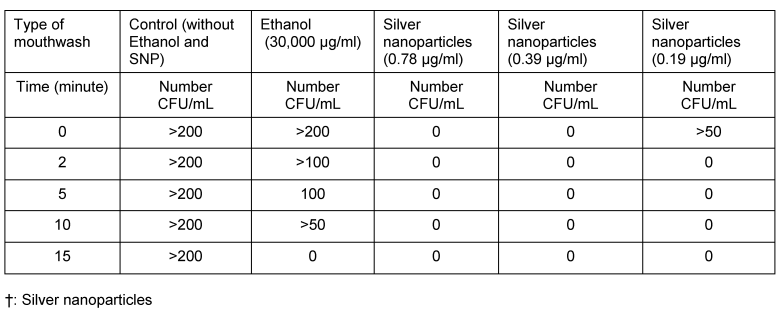
4 Discussion
Many investigative studies have documented the inhibition of plaque growth and the reduction of bacterial acid formation by the use of antibacterial agents added to mouthrinses or toothpaste preparations [32]. According to their chemical characteristics, available mouth rinses commercially contain cationic, anionic and nonionic active ingredients, which at either a higher or lower extent alter the bacterial membrane function. Among the cationic agents, chlorhexidine and some divalent metal ions like Cu+2, Zn+2, and Sn+2 are most widely used [9]. It has been demonstrated that Streptococcus mutans are unable to acquire the nutrients necessary for its survival and reproduction [35]. May be the metal iron can modify the functional of the cell membrane and also the enzyme activity of cell [16]. Modifying the different zinc salts and its derivatives with the new formulation are useful to control oral plaque and gingival bleeding [33]. Dobl and Nossek in 1990 [10] showed that the 0.2% and 0.4% of zinc chloride mouthrinses have antibacterial activity against dental plaque especially Streptococcus flora [32]. To investigate antimicrobial activity of SNP solution against microorganisms, we measured the MIC and MBC (MFC), and then challenge test was done to compare antimicrobial effects of ethanol of 30,000 µg/ml and SNP (different concentrations). Eldridge and colleagues in 1998 [14] found no difference between the commercial alcohol-based chlorhexidine 0.12% and the alcohol-free chlorhexidine 0.12% through both in vitro and in vivo studies. The commercially available mouthwash solution that was tested in this study contains 30,000 µg/ml of alcohol. Mouthwashes that contain alcohol, are contraindicated in special patients who had mucositis and other immunocompromised [36]. Winn and colleagues found relationship between oral cancer and alcohol-based mouthwashes. The risk of oral cancer increased by 40–60%, after adjusting for comparison other risk factors, such as tobacco and alcohol consumption [39]. Hence, it’s important to avoid the use of alcoholic mouthwash. Gram-negative bacteria, such as Klebsiella pneumoniae and Pseudomonas aeruginosa, and Gram-positive bacteria, such as Methicillin-resistant Staphylococcus aureus that frequently colonize the oral cavity of hospitalized patients [25], have emerged as causes of nosocomial pneumonia. This has stimulated the search for preventive and therapeutic measures to minimize oral and respiratory colonization by the simple use of a broad-spectrum antiseptic mouthwash pre-operatively or pre-intubation [2].
In this study, SNP killed both investigated Gram-negative bacteria faster than S. aureus despite the fact that MIC of SNP for S. aureus was lower than E. coli, with a broad range between MIC and MBC of SNP for S. aureus (MIC=1.56, MBC=12.5). These results are similar to reported results by Jain et al. [21], they reported that Gram-negative bacteria such as E. coli and P. aeruginosa were killed at MIC (6.25 µg/ml) of SNP faster than Gram-positive bacteria such as S. aureus and Bacillus subtilis at MIC (12.5 µg/ml) of SNP also MBC value could not be determined because SNP was found to be bacteriostatic even at the highest concentration available for testing, i.e., 50 µg/ml. Although MIC of PVP stabilized SNP for S. aureus and E. coli was 5 µg/ml and 10 µg/ml respectively; all viable cells of E.coli were inhibited by SNP solution of 10 and 20 µg/ml faster than S. aureus [8]. Previous studies indicated that S. aureus is less susceptible to SNP in comparison with E. coli and P. aeruginosa [31]. It is determined that antimicrobial effects of SNP also depend on type of microbial strain. Different strains of E. coli, Bacillus subtilis and S. aureus showed variation in the SNP established antimicrobial effects [34]. Others reported similar results, too [21]. They showed that MIC values and time requirement to achieve inhibitory effect of SNP for S. aureus are different from S. epidermidis. Our results corroborate these findings because MIC and MBC values of SNP for both Gram-positive bacteria (S. mutans and S. aureus) are different. S. mutans was killed faster than S. aureus by mouthwash containing SNP with MIC and two lower concentrations. This is an important result, because very low concentrations of SNP can be used for prevention of dental caries in mouthwash but it requires more experiments. Hernandez-Sierra showed that MIC and MBC for silver nanoparticles (The average size of nanoparticles was 25 nm.) were 4.86 µg/ml and 6.25 µg/ml. They reported that silver nanoparticles inhibit S. mutans at lower concentration than gold or zinc nanoparticles [18]. In previous studies, copper and zinc have been used as an antimicrobial factor in mouthwash [6]. Burguera-Pascu et al. used zinc salts as rinsing solution and they reported a high effectiveness of the Zn salts on S. mutans [6]. Mouthwashes containing very low zinc compounds have shown high antimicrobial effects on strains of Streptococcus in mouth [10]. We used colloidal solution of SNP that was very effective toward C. albicans. MIC and MBC values of SNP for C. albicans were 0.78 and 1.56 µg/ml respectively. In vitro study showed that the experimental mouthwash, while being free of alcohol and containing reduced concentration of SNP was shown to be efficacious in inhibiting bacterial and candidal activity. These values are comparable to those obtained by Kokura et al. [22]. They reported that SNP of 1 µg/ml showed sufficient antimicrobial efficacy against mixed bacteria (S. aureus, E. coli, P. aeroginusa) and mixed fungi (Candida albicans, Aspergillus niger, Penicillium citrium, Aureobasidium pullulans) in addition, previous studies showed that hybrid silver nanoparticles (size 3–7 nm) loaded on SiO2 nanoparticles inhibited a range of standard fungi at concentration of 1 µg/ml [30]. It has been determined that antimicrobial effects of SNP depend on size of particles. 25 nm sizes SNP had lower MIC than SNP with size more than 25 nm. MIC of this SNP (25 nm) was 1.69–13.5 µg/ml [29]. The MIC results obtained from 25 nm particles are comparable to those obtained by the present research, where as SNP suspensions containing 10–40 nm particles were used, also MIC and MBC values obtained our study is near to those reported by Jain et al. [21]. They used SNP suspension containing 7–20 nm particles that these SNP had MIC from 6.25 to 12.5 µg/ml. In an another study, 24 nm SNP had MIC between 1.2 and 1.7 µg/mL against clinical isolates such as E. coli, S. aureus and P. aeroginusa [24].
In conclusion, our study showed that SNP has high antimicrobial properties against C. albicans and other common bacteria and the novel mouthwash (containing SNP and alcohol free) may serve as a convenient alternative mouthwash for immunocompromised cancer patients and for preoperative patients at high risk for nosocomial pneumonia. The low concentration of SNP may minimize the unpleasant taste and also reduce toxicity. Furthermore, being alcohol-free makes it non-irritant and comfortable to use for patients with sensitive or inflamed mucosa. Yet, biologcal and environmental effects of SNP must be studied further before SNP may be considered to be added into a commercially available antimicrobial mouthwash.
Notes
Competing interests
The authors declare that they have no competing interests.
References
[1] Abu-Elteen KH, Abu-Alteen RM. The prevalence of Candida albicans populations in the mouths of complete denture wearers. New Microbiol. 1998 Jan;21(1):41-8.[2] Baxter AD, Allan J, Bedard J, Malone-Tucker S, Slivar S, Langill M, Perreault M, Jansen O. Adherence to simple and effective measures reduces the incidence of ventilator-associated pneumonia. Can J Anaesth. 2005 May;52(5):535-41. DOI: 10.1007/BF03016535
[3] Belazi M, Velegraki A, Koussidou-Eremondi T, Andreadis D, Hini S, Arsenis G, Eliopoulou C, Destouni E, Antoniades D. Oral Candida isolates in patients undergoing radiotherapy for head and neck cancer: prevalence, azole susceptibility profiles and response to antifungal treatment. Oral Microbiol Immunol. 2004 Dec;19(6):347-51. DOI: 10.1111/j.1399-302x.2004.00165.x
[4] Bodey G, Bueltmann B, Duguid W, Gibbs D, Hanak H, Hotchi M, Mall G, Martino P, Meunier F, Milliken S, et al. Fungal infections in cancer patients: an international autopsy survey. Eur J Clin Microbiol Infect Dis. 1992 Feb;11(2):99-109. DOI: 10.1007/BF01967060
[5] Brul S, Coote P. Preservative agents in foods. Mode of action and microbial resistance mechanisms. Int J Food Microbiol. 1999 Sep 15;50(1-2):1-17. DOI: 10.1016/S0168-1605(99)00072-0
[6] Burguera-Pascu M, Rodríguez-Archilla A, Baca P. Substantivity of zinc salts used as rinsing solutions and their effect on the inhibition of Streptococcus mutans. J Trace Elem Med Biol. 2007;21(2):92-101. DOI: 10.1016/j.jtemb.2006.12.003
[7] Chipley JR. Sodium benzoate and benzoic acid. In: Branen AL, Davidson PM, eds. Antimicrobials in foods. New York, NY: M. Decker; 1983. p. 11-35.
[8] Cho KH, Park JE, Osaka T, Park SG. The study of antimicrobial activity and preservative effects of nanosilver ingredient. Electrochim Acta. 2005; 51:956-60. DOI: 10.1016/j.electacta.2005.04.071
[9] Dahlman P. Antimicrobial agents and treatments with special reference to dental caries. Malmo: Malmo University, Faculty of Odontology, Department of Cariology; May 2005.
[10] Dobl P, Nossek H. Einfluss von Zinkchloridmundspülungen auf kariesinduzierende Plaquestreptokokken. 2. Mitteilung: In vivo Untersuchungen zur antibakteriellen Wirkung von Zinkchlorid auf die Gesamtstreptokokkenflora der Zahnplaque [The effect of zinc chloride mouthwashes on caries-inducing plaque streptococci. 2. In vivo studies of the antibacterial effect of zinc chloride on the total streptococcal flora of the dental plaque]. Zahn Mund Kieferheilkd Zentralbl. 1990;78(5):393-6.
[11] Double-blind trial comparing two dosage schedules of beclomethasone dipropionate aerosol in the treatment of chronic bronchial asthma. Preliminary report of the Brompton Hospital-Medical Research Council Collaborative Trial. Lancet. 1974 Aug 10;2(7876):303-7.
[12] Efficacy of Antimicrobial Preservation. In: British Pharmacopeia. Version 7, Volume 3, Appendix XVI C. 2003. p. 136.
[13] Efficacy of preservation of non-eye area water-miscible cosmetic and toiletry formulations (chapter 15). In: AOAC Official Methods of Analysis; 2000. p. 3-5.
[14] Eldridge KR, Finnie SF, Stephens JA, Mauad AM, Munoz CA, Kettering JD. Efficacy of an alcohol-free chlorhexidine mouthrinse as an antimicrobial agent. J Prosthet Dent. 1998 Dec;80(6):685-90. DOI: 10.1016/S0022-3913(98)70056-3
[15] Epstein JB, Hancock PJ, Nantel S. Oral candidiasis in hematopoietic cell transplantation patients: an outcome-based analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003 Aug;96(2):154-63. DOI: 10.1016/S1079-2104(03)00296-8
[16] Giertsen E. Effects of mouthrinses with triclosan, zinc ions, copolymer, and sodium lauryl sulphate combined with fluoride on acid formation by dental plaque in vivo. Caries Res. 2004 Sep-Oct;38(5):430-5. DOI: 10.1159/000079623
[17] Handa O, Kokura S, Adachi S, Takagi T, Naito Y, Tanigawa T, Yoshida N, Yoshikawa T. Methylparaben potentiates UV-induced damage of skin keratinocytes. Toxicology. 2006 Oct 3;227(1-2):62-72. Epub 2006 Jul 28. DOI: 10.1016/j.tox.2006.07.018
[18] Hernández-Sierra JF, Ruiz F, Pena DC, Martínez-Gutiérrez F, Martínez AE, Guillén Ade J, Tapia-Pérez H, Castañón GM. The antimicrobial sensitivity of Streptococcus mutans to nanoparticles of silver, zinc oxide, and gold. Nanomedicine. 2008 Sep;4(3):237-40. DOI: 10.1016/j.nano.2008.04.005
[19] Holladay R, Moeller W, Mehta D, Brooks J, Roy R, Mortenson M. Silver/water, silver gels and silver-based compositions; and methods for making and using the same. European Patent Office; 2006. Applicationnumber: W02005US47699 20051230.
[20] Hu M, Wang J, Cai J, Wu Y, Wang X. [Analysis of sodium benzoate biotoxicity by atomic force microscope]. Sheng Wu Gong Cheng Xue Bao [Chinese Journal of Biotechnology]. 2008 Aug;24(8):1428-32. DOI: 10.1016/S1872-2075(08)60064-3
[21] Jain J, Arora S, Rajwade JM, Omray P, Khandelwal S, Paknikar KM. Silver nanoparticles in therapeutics: development of an antimicrobial gel formulation for topical use. Mol Pharm. 2009 Sep-Oct;6(5):1388-401. DOI: 10.1021/mp900056g
[22] Kokura S, Handa O, Takagi T, Ishikawa T, Naito Y, Yoshikawa T. Silver nanoparticles as a safe preservative for use in cosmetics. Nanomedicine. 2010 Aug;6(4):570-4. DOI: 10.1016/j.nano.2009.12.002
[23] Krebs HA, Wiggins D, Stubbs M, Sols A, Bedoya F. Studies on the mechanism of the antifungal action of benzoate. Biochem J. 1983 Sep 15;214(3):657-63.
[24] Martínez-Gutierrez F, Thi EP, Silverman JM, de Oliveira CC, Svensson SL, Vanden Hoek A, Sánchez EM, Reiner NE, Gaynor EC, Pryzdial EL, Conway EM, Orrantia E, Ruiz F, Av-Gay Y, Bach H. Antibacterial activity, inflammatory response, coagulation and cytotoxicity effects of silver nanoparticles. Nanomedicine. 2012 Apr;8(3):328-36. DOI: 10.1016/j.nano.2011.06.014
[25] Martins ST, Moreira M, Furtado GH, Marino CG, Machado FR, Wey SB, Medeiros EA. Application of control measures for infections caused by multi-resistant gram-negative bacteria in intensive care unit patients. Mem Inst Oswaldo Cruz. 2004 May;99(3):331-4. DOI: 10.1590/S0074-02762004000300017
[26] McCann D, Barrett A, Cooper A, Crumpler D, Dalen L, Grimshaw K, Kitchin E, Lok K, Porteous L, Prince E, Sonuga-Barke E, Warner JO, Stevenson J. Food additives and hyperactive behaviour in 3-year-old and 8/9-year-old children in the community: a randomised, double-blinded, placebo-controlled trial. Lancet. 2007 Nov 3;370(9598):1560-7. DOI: 10.1016/S0140-6736(07)61306-3
[27] Odds FC. Candida and candidiasis. A review and bibliography. 2nd ed. London: Bailliere Tindall; 1988. p. 117.
[28] Pal S, Tak YK, Song JM. Does the antibacterial activity of silver nanoparticles depend on the shape of the nanoparticle? A study of the Gram-negative bacterium Escherichia coli. Appl Environ Microbiol. 2007 Mar;73(6):1712-20. DOI: 10.1128/AEM.02218-06
[29] Panacek A, Kvítek L, Prucek R, Kolar M, Vecerova R, Pizúrova N, Sharma VK, Nevecna T, Zboril R. Silver colloid nanoparticles: synthesis, characterization, and their antibacterial activity. J Phys Chem B. 2006 Aug;110(33):16248-53. DOI: 10.1021/jp063826h
[30] Park HJ, Kim HJ, Kim SH, Oh SD, Choi SH. Radiolytic: synthesis of hybrid silver nanoparticles and their biobehavior. Key Eng Mater. 2007;342-343:897-900. DOI: 10.4028/www.scientific.net/KEM.342-343.897
[31] Petica A, Gavriliu S, Lungu M, Buruntea N, Panzaru C. Colloidal silver solutions with antimicrobial properties. Mater Sci Eng B. 2008;152:22-7. DOI: 10.1016/j.mseb.2008.06.021
[32] Phan TN, Buckner T, Sheng J, Baldeck JD, Marquis RE. Physiologic actions of zinc related to inhibition of acid and alkali production by oral streptococci in suspensions and biofilms. Oral Microbiol Immunol. 2004 Feb;19(1):31-8. DOI: 10.1046/j.0902-0055.2003.00109.x
[33] Roldán S, Herrera D, O'Connor A, González I, Sanz M. A combined therapeutic approach to manage oral halitosis: a 3-month prospective case series. J Periodontol. 2005 Jun;76(6):1025-33. DOI: 10.1902/jop.2005.76.6.1025
[34] Ruparelia JP, Chatterjee AK, Duttagupta SP, Mukherji S. Strain specificity in antimicrobial activity of silver and copper nanoparticles. Acta Biomater. 2008 May;4(3):707-16. DOI: 10.1016/j.actbio.2007.11.006
[35] Scheie AA. The role of antimicrobials. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford: Blackwell Munksgard; 2003.
[36] Sreenivasan PK, Mattai J, Nabi N, Xu T, Gaffar A. A simple approach to examine early oral microbial biofilm formation and the effects of treatments. Oral Microbiol Immunol. 2004 Oct;19(5):297-302. DOI: 10.1111/j.1399-302x.2004.00158.x
[37] Webb BC, Thomas CJ, Whittle T. A 2-year study of Candida-associated denture stomatitis treatment in aged care subjects. Gerodontology. 2005 Sep;22(3):168-76.
[38] Wei D, Sun W, Qian W, Ye Y, Ma X. The synthesis of chitosan-based silver nanoparticles and their antibacterial activity. Carbohydr Res. 2009 Nov;344(17):2375-82. DOI: 10.1016/j.carres.2009.09.001
[39] Winn DM, Blot WJ, McLaughlin JK, Austin DF, Greenberg RS, Preston-Martin S, Schoenberg JB, Fraumeni JF Jr,. Mouthwash use and oral conditions in the risk of oral and pharyngeal cancer. Cancer Res. 1991 Jun;51(11):3044-7.
[40] Woo SB, Sonis ST, Monopoli MM, Sonis AL. A longitudinal study of oral ulcerative mucositis in bone marrow transplant recipients. Cancer. 1993 Sep;72(5):1612-7. DOI: 10.1002/1097-0142(19930901)72:5<1612::AID-CNCR2820720520>3.0.CO;2-Q
[41] Worthington HV, Clarkson JE. Prevention of oral mucositis and oral candidiasis for patients with cancer treated with chemotherapy: cochrane systematic review. J Dent Educ. 2002 Aug;66(8):903-11.
[42] Xue B, Wang HF, Xu LH, Sun HF, Liu YF, Peng SX, Liu KX, Guo ZY. Benzoate drived DNA adduction and its decay in mice measured by AMS. Nucl Instrum Methods Phys Res B. 2004;223-224:765-9. DOI: 10.1016/j.nimb.2004.04.142
Erratum
The spelling of the first author’s name (originally Marzieh Fattahi Dolat Abadi) as well as the determination of the personal name heading (originally Abadi) has been corrected.




