[Ein Zystadenom imitierende primäre Hydatidenzyste im Eierstock: Ein seltener Fallbericht]
Ensiyeh Bahadoran 1Fatemeh Samieerad 2
Simindokht Molaverdikhani 3
Saeideh Gholamzadeh Khoei 4
1 Student Research Committee, Qazvin University of Medical Sciences, Qazvin, Iran
2 Department of Pathobiology, Faculty of Medical School, Qazvin University of Medical Sciences Qazvin, Kowsar Medical and Educational Center, Qazvin, Iran
3 Kowsar Clinical Research Development Unit, Qazvin University of Medical Sciences, Qazvin, Iran
4 Medical Microbiology Research Center, Qazvin University of Medical Sciences, Qazvin, Iran
Zusammenfassung
Hintergrund: Echinokokkuszysten (EZ) sind Zoonosen, die hauptsächlich durch Echinococcus granulosus verursacht werden. Echinokokkuszysten im Eierstock sind eine seltene Erkrankung mit unterschiedlichen, unspezifischen Präsentationen. In diesem Bericht stellen wir einen seltenen Fall einer primären Echinokokkuszyste im Eierstock vor.
Kasuistik: Eine 47-jährige Frau mit chronischen Bauchschmerzen und einer gefüllten linken Becken wurde in die Geburtsklinik des Kowsar-Krankenhauses in Qazvin überwiesen. Die abdominale Sonographie zeigte eine zystische Masse, die zunächst auf ein Zystadenom hindeutete. Die Tumormarkerwerte lagen aber im normalen Bereich. Nach chirurgischer Resektion zeigte die histopathologische Untersuchung eine zystische außen und innen glatte Masse mit Abmessungen von 10×6×3 cm, einer Wanddicke von 0,3 cm und mehreren Stücken unregelmäßigen grauen membranösen Gewebes. Die Patientin erhielt 3 Monate nach der Operation eine Behandlung mit Albendazol; die 6-monatige Nachuntersuchung per Ultraschall ergab keine Anzeichen für ein Rezidiv.
Schlussfolgerung: Echinokokkuszysten zeigen unspezifische Symptome. Radiologen, Pathologen und Chirurgen sollten EZ als differenzialdiagnostische Möglichkeit für jede zystische Masse im Beckenraum in Betracht ziehen, insbesondere in endemischen Gebieten. Chirurgische Resektion und die Verabreichung von Albendazol sind die bevorzugten Behandlungen.
Schlüsselwörter
Hydatidenzyste, primär, Eierstock, Echinococcosis
Introduction
Anthropozoonosis, known as hydatid illness, is caused by Echinococcus (E.) species tapeworms in the larval stages. E. granulosus, E. multilocularis, E. oligarthrus, and E. vogeli are the species involved in the disease, with E. granulosus being the most prevalent, accounting for 95% of cyst formations [1], [2]. In the intestines of carnivores, such as dogs (the parasite's definitive host), the worm attaches to the mucosa using hooklets. The eggs of the parasite are excreted in the feces of carnivores and are later ingested by herbivores like sheep and cattle, acting as the intermediate hosts for the parasite. Following this, the larva penetrates the intestinal wall and migrates throughout the body via the bloodstream [3], [4]. When the definitive host consumes the intermediate host's viscera, its life cycle is completed [5]. Humans can be incidental hosts [6][6], and can become infected by eating unwashed vegetables, drinking contaminated water, touching infected soil, or being near pet dogs [7].
Hydatid cysts (HC) are most frequently found in the liver and lungs [8]. Pulmonary HC grow more quickly than liver HC because the lungs have a softer consistency than the liver. Furthermore, because children’s lung tissues are more elastic than those of adults, HC in children grow larger and faster [9]. Approximately 0.2% to 2.25% of HC cases involve the ovary. It can appear in a primary or secondary form and shares morphological similarities with other areas. About twenty instances of primary ovarian HC have been documented [10]. The secondary form is more prevalent and is associated with multiorgan HC, lungs, or liver echinococcosis [10]. The pericyst, comprising the host’s inflammatory tissue, exocyst, and endocyst, where the scolecs and proligere membrane are generated, makes up the cyst's typical structure [5].
Based on its location, size, and host immunological response, this disease can exhibit different clinical presentations and complications. Symptoms can range from asymptomatic – due to the slow-growing nature of cysts in most cases – to anaphylactic shock due to cyst rupture or fistulization into adjacent organs [4], [11].
Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) are the most frequently used imaging techniques for the diagnosis and follow-up of patients with HC. Ultrasound is used for HC staging and treatment planning [12], [13]. Based on the sonogram, cystic echinococcosis (CE) is divided into three classes according to the state of activity: active (CE1 and CE2) with clear contents and water-lily sign; transitional (CE3), with the immune system or drugs compromising the cyst; and inactive (CE4 and CE5), with calcification of the cyst wall [12]. Although ultrasound cannot provide a definitive answer, it is a viable option for screening, post-treatment monitoring, and cyst staging [14]. The cyst size, number, and local problems can all be observed on a CT scan, along with osseous organ involvement, and the presence of calcifications. In cases of biliary or neurological involvement, and to distinguish HC from neoplasms, MRI is preferred [4][4]. An enzyme-linked immunosorbent assay (ELISA) test in the active stages of the disease may be informative [15]. Pharmacological treatment, surgery, endoscopic interventional treatment, and subsequent minimally invasive techniques are some therapeutic approaches to hepatic hydatid disease [13].
Because HC is a rare entity, it should be considered in the differential diagnosis of any cystic mass in the pelvic cavity, especially in endemic areas, to provide optimal treatment before surgery and prevent accidental rupture of the cyst during surgery. In this paper, we present a rare case of an ovarian hydatid cyst in a 47-year-old woman and describe its management.
Case presentation
Informed consent was obtained from the patient before enrollment in the study. A 47-year-old woman presenting with six months of chronic abdominal pain and left hemipelvic fullness without radiation was referred to the Obstetrics Clinic of Kowsar Hospital of Qazvin, Iran, in 2023. She had a history of three vaginal deliveries, normal menstrual cycles, no history of weight change or abdominal surgery, and no history of HC in herself or her family. She is a retired teacher who lives in the urban Qazvin. She had no contact with animals but occasionally traveled to rural areas. Physical examination of the abdomen revealed deep tenderness of the right suprapubic region with no palpable mass or skin abnormalities. No other abnormalities were detected on systemic or gynecological examinations.
Abdominopelvic sonography revealed a cystic mass with a lobular margin, and dimensions of 70×95×75 mm in the left hemipelvis, which lacked solid, nodulation, and calcification components, primarily suggesting a cyst adenoma. Chest imaging was normal (Figure 1 [Fig. 1]). The levels of tumor markers, including cancer antigen (CA)-125, carcinoembryonic antigen (CEA), alpha-fetoprotein (AFP), and beta-human chorionic gonadotropin (beta-hCG) were within normal limits.
Figure 1: Cystic mass with a lobular margin shown by abdominopelvic sonography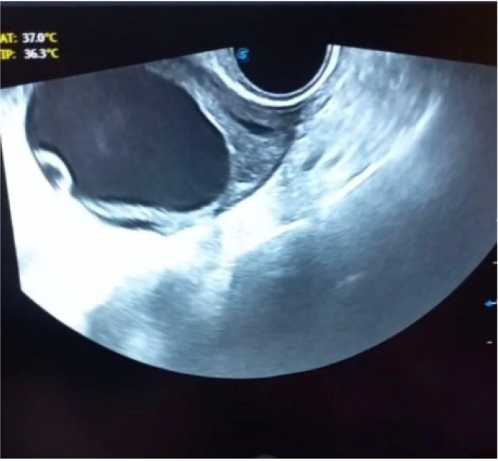
She underwent resection of the cystic lesion. On gross pathological examination, a cystic mass measuring 10×6×3 cm, with smooth external and internal aspects, wall thickness of 0.3 cm, and multiple pieces of irregular gray membranous tissue, were observed (Figure 2 [Fig. 2]). Albendazole treatment was initiated and continued for three months. The post-surgical course was uneventful and the follow-up sonogram showed no signs of recurrence after 6 months.
Figure 2: Ovarian hydatid cyst revealed fragmented acellular laminated layer, protoscolex admixed with necrotic material (400×, Hematoxylin & Eosin)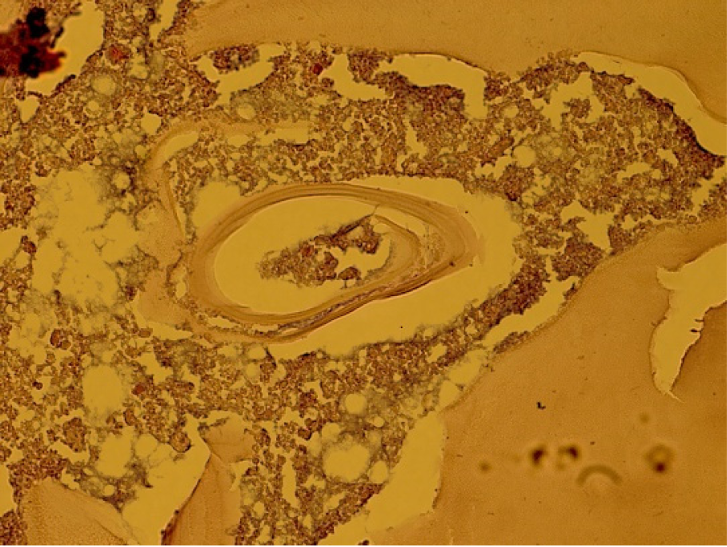
Discussion
HC is a global parasitic ailment, prevalent in numerous regions where sheep and cattle are raised, with endemic occurrences. In various regions of North and East Africa, Europe, Asia, the Middle East, and South America, the illness is severely endemic [16]. Ovarian hydatid cysts are rare, with about two-thirds of cysts occurring as primary cysts; the majority of them have been reported in countries known as endemic zones, such as India, Iran, and Turkey [10]. Approximately four to five weeks after being infected with E. granulosus through the gastrointestinal route, larvae are released in the intestine. They then breach the epithelium, reaching the lamina propria and disseminating to other organs through lymphatic and blood circulation. They develop into hydatid cysts over the course of about five to fifteen years, eventually manifesting symptoms [11], [17]. HC are more prevalent in females than in males, as they have more contact with domestic animals and infected products [18]. Ovarian HC has been diagnosed at ages ranging from 12 to 76 years [10]. Consistent with this, our patient was a 47-year-old female, from an endemic area, who occasionally traveled to rural areas and was possibly infected through contaminated water or vegetables.
Involvement of pelvic organs is highly uncommon, given that the cyst often remains asymptomatic for an extended period before being diagnosed [3]. Symptoms typically arise in cases of cyst infections, upon cyst rupture, or due to the compression of adjacent organs or tissues by the cyst [19]. For ovarian HC, symptoms such as abdominal pain and distention [20], frequent urination [3] or urinary obstruction [21], pelvic pain or discomfort [22], postmenopausal metrorrhagia [23], occasional dysmenorrhea [24], and amenorrhea [25] have been reported. Our patient had hemi-pelvic fulness in addition to the most common symptom, i.e., abdominal pain.
Rupture can be triggered by trauma or may happen spontaneously because of elevated pressure in the cystic fluid. Key risk factors that make rupture more likely include a younger age, cyst diameter exceeding 10 cm, and the cyst being situated close to the surface [26]. In 16–25% of cases, rupture occurs, and in those situations, the rate of a severe reaction ranges from 1 to 12.5% [27]. It is possible to eliminate daughter cysts and lower the danger of allergic reactions by using solutions containing 0.5% cetrimide, 15% hypertonic saline, 1% silver nitrate, and sodium hypochlorite [28]. Cautious exposure and drainage have proven to be a safe and reliable treatment for peritoneal cysts strongly attached to intraperitoneal viscera. To avert secondary hydatidosis and allergic reactions, it is essential to isolate the abdominal cavity using gauze soaked in a 20% hypertonic saline solution [20].
Ultrasound, CT scan, MRI, and laboratory tests, are used to make the diagnosis. Only histological evidence can verify a final diagnosis [27]. The accuracy of serological testing can be affected by the size, location, and clinical phases of CE. The sensitivity of serological tests varies depending on the illness stage; for patients with inactive or early cystic stages, it is around 50%, while for those with active cysts, it is greater [29]. Our patient had one inactive cyst, with CE stages 4 and 5. A chest radiograph and abdominopelvic sonographic exam were performed to check for potential HCs in the liver or lung. In our case, neither the liver nor the lungs showed any signs of involvement.
In our case, the HC mimicked an ovarian cyst adenoma, which can also be asymptomatic, and when large, they present with abdominal and pelvic pain [30]. However, negative tumor markers ruled out this diagnosis.
Surgery, either radical or conservative, is the most effective treatment for hydatid cysts, but it cannot prevent recurrence. Performing a complete resection is necessary to prevent the cyst from rupturing perioperatively. Treatment with benzimidazole compounds, such as albendazole or mebendazole, and the recently developed PAIR procedure (puncture-aspiration-injection-re-aspiration), which destroys the cyst’s germinal layer, offer additional treatment options for HC cases [31].
Conclusions
Ovarian HC is a rare entity that occurs primarily without the involvement of the liver or lungs. This disease has different presentations, and non-specific radiological and laboratory findings. Radiologists, pathologists, and surgeons should be aware of this disease and consider it as a differential diagnosis for any cystic mass in the pelvic cavity, particularly in endemic areas. Surgical resection of the cyst is the gold standard of therapy, and with benzimidazole compounds before and after surgery, progression and recurrence can be eliminated.
Notes
Competing interests
The authors declare that they have no competing interests.
Acknowledgment
We give our special thanks to the Clinical Research Center of Kowsar Hospital affiliated with Qazvin University of medical sciences.
Authors’ ORCID
- Ensiyeh Bahadoran: 0000-0001-8299-1466
- Fatemeh Samieerad: 0000-0001-6091-4347
- Simindokht Molaverdikhani: 0000-0001-6602-0854
- Saeideh Gholamzadeh Khoei: 0000-0003-2675-9392
References
[1] Kazzaz R, Nashed D, Sattout GIA, Issa N, Aldakhil A, Bitar O, Danial AK. Laparoscopic management of a primary gallbladder hydatid cyst with daughter cysts in the common bile duct: Case report. Ann Med Surg (Lond). 2022 Aug;80:104165. DOI: 10.1016/j.amsu.2022.104165[2] Eskandari F, Mohaghegh MA, Mirzaei F, Ghomashlooyan M, Hejazi SH. Molecular characteristics of Echinococcus granulosus strains isolated from Iranian camel using high resolution melting analysis of atp6 and cox1 genes . Avicenna J Clin Microbiol Infect. 2017; 5(2):14-9. DOI: 10.34172/ajcmi.2018.03
[3] Mohammed AA, Arif SH. Hydatid cyst of the ovary - a very rare type of cystic ovarian lesion: A case report. Case Rep Womens Health. 2021 Jul;31:e00330. DOI: 10.1016/j.crwh.2021.e00330
[4] Abbasi B, Akhavan R, Ghamari Khameneh A, Darban Hosseini Amirkhiz G, Rezaei-Dalouei H, Tayebi S, Hashemi J, Aminizadeh B, Darban Hosseini Amirkhiz S. Computed tomography and magnetic resonance imaging of hydatid disease: A pictorial review of uncommon imaging presentations. Heliyon. 2021 May;7(5):e07086. DOI: 10.1016/j.heliyon.2021.e07086
[5] Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;20(3):795-817. DOI: 10.1148/radiographics.20.3.g00ma06795
[6] Kouzegaran S, Sabertanha A. Accidental discovery of a hydatid cyst with primary presentation in an unusual location: a case report. J Surg Trauma. 2016;4(2):27-9.
[7] Biswas B, Mondal P, Das T, Keditsu T. Rare coexisting primary hydatid cyst and mucinous cyst adenoma of right ovary. Indian J Clin Prac. 2013;24(5):469-71.
[8] Sachar S, Goyal S, Goyal S, Sangwan S. Uncommon locations and presentations of hydatid cyst. Ann Med Health Sci Res. 2014 May;4(3):447-52. DOI: 10.4103/2141-9248.133476
[9] Shahriarirad R, Erfani A, Ebrahimi K, Rastegarian M, Eskandarisani M, Ziaian B, Sarkari B. Hospital-based retrospective analysis of 224 surgical cases of lung hydatid cyst from southern Iran. J Cardiothorac Surg. 2023 Jul;18(1):204. DOI: 10.1186/s13019-023-02327-w
[10] Lozneanu L, Anca Balan R, Giuşcă SE, Căruntu ID, Amălinei C, Grigoraş A. Ovarian hydatid cyst-systematic review of clinicopathological and immunohistochemical characteristics of an unusual entity. Rom J Morphol Embryol. 2019;60(3):751-9.
[11] Samiee-Rad F, Emami A. An Iranian man with increased thigh mass due to a hydatid cyst. GMS Hyg Infect Control. 2020 Aug 20;15:Doc20. DOI: 10.3205/dgkh000355
[12] Agudelo Higuita NI, Brunetti E, McCloskey C. Cystic Echinococcosis. J Clin Microbiol. 2016 Mar;54(3):518-23. DOI: 10.1128/JCM.02420-15
[13] Botezatu C, Mastalier B, Patrascu T. Hepatic hydatid cyst - diagnose and treatment algorithm. J Med Life. 2018;11(3):203-9. DOI: 10.25122/jml-2018-0045
[14] Stojkovic M, Rosenberger K, Kauczor HU, Junghanss T, Hosch W. Diagnosing and staging of cystic echinococcosis: how do CT and MRI perform in comparison to ultrasound? PLoS Negl Trop Dis. 2012;6(10):e1880. DOI: 10.1371/journal.pntd.0001880
[15] Mohammed AA, Arif SH. Surgical excision of a giant pedunculated hydatid cyst of the liver. J Surg Case Rep. 2019 Jul;2019(7):rjz208. DOI: 10.1093/jscr/rjz208
[16] Grosso G, Gruttadauria S, Biondi A, Marventano S, Mistretta A. Worldwide epidemiology of liver hydatidosis including the Mediterranean area. World J Gastroenterol. 2012 Apr;18(13):1425-37. DOI: 10.3748/wjg.v18.i13.1425
[17] Gattani R, Malhotra G, Deshpande SG, Ramteke H, Nayak K, Salwan A, et al. Asymptomatic incidental primary pelvic hydatid cyst in a post-menopausal woman: A case report. Med Sci. 2023 Jan 1;27(131):1-5. DOI: 10.54905/disssi/v27i131/e12ms2609.
[18] Farazi A, Zarinfar N, Kayhani F, Khazaie F. Hydatid Disease in the Central Region of Iran: A 5-year Epidemiological and Clinical Overview. Cent Asian J Glob Health. 2019;8(1):364. DOI: 10.5195/cajgh.2019.364
[19] Rawla P, Sunkara T, Muralidharan P, Raj JP. An updated review of cystic hepatic lesions. Clin Exp Hepatol. 2019 Mar;5(1):22-9. DOI: 10.5114/ceh.2019.83153
[20] Rabiee S, Fallah N, Rabiee S, Fallah M. Primary disseminated hydatid cysts in a 14-year-old girl: a case report. Acta Med Iran. 2017;55(11):726-9.Dharsandia MV, Soni ST, Vegad MM. Ovarian hydatid cyst in pediatric patient commencing as ovarian tumor: a rare site of echinococcosis. Int J Prev Med. 2012 Dec;3(12):897-9. DOI: 10.4103/2008-7802.104863
[21] Dharsandia M V, Soni ST, Vegad MM. Ovarian hydatid cyst in pediatric patient commencing as ovarian tumor: a rare site of echinococcosis. Int J Prev Med. 2012;3(12):897. DOI: 10.4103/2008-7802.104863.
[22] Fatnassi R, Turki E, Majdoub W, Hammami S, Hajji M. Primary ovarian hydatid cyst: a case report and review of literature. Insights Reprod Med. 2017;1(1):5.
[23] Alonso García ME, Suárez Mansilla P, Mora Cepeda P, Bayón Álvarez E, Alvarez Colomo C, González Martín JI. Ovarian hydatid disease. Arch Gynecol Obstet. 2014 May;289(5):1047-51. DOI: 10.1007/s00404-013-3096-1
[24] Zhao Q, Luo J, Zhang Q, Leng T, Yang L. Laparoscopic surgery for primary ovarian and retroperitoneal hydatid disease: A case report. Medicine (Baltimore). 2018 Jan;97(3):e9667. DOI: 10.1097/MD.0000000000009667
[25] Ray S, Gangopadhyay M. Hydatid cyst of ovary- a rare entity. J Turk Ger Gynecol Assoc. 2010;11(1):63-4.
[26] Yilmaz M, Akbulut S, Kahraman A, Yilmaz S. Liver hydatid cyst rupture into the peritoneal cavity after abdominal trauma: case report and literature review. Int Surg. 2012;97(3):239-44. DOI: 10.9738/CC116.1
[27] Kulwal AL, Vakharia D. Ovarian hydatid cyst as a unique cause for obstructed labo – case report. Bharati Vidyapeeth Med J. 2023;3(1). DOI: 10.56136/BVMJ/2022_00100.
[28] Akinci ÖF, Karaoǧlanoǧlu M, Bozkurt MS, Gözaydin L, Ziylan SZ. In vitro efficacy of different chemical substances on hydatid cyst components. Turk J Med Sci. 2011;41(1):17-23. DOI: 10.3906/sag-1003-707.
[29] Griffin DO, Donaghy HJ, Edwards B. Management of serology negative human hepatic hydatidosis (caused by Echinococcus granulosus) in a young woman from Bangladesh in a resource-rich setting: A case report. IDCases. 2014;1(2):17-21. DOI: 10.1016/j.idcr.2014.02.003
[30] Abduljabbar HS, Bukhari YA, Al Hachim EG, Alshour GS, Amer AA, Shaikhoon MM, Khojah MI. Review of 244 cases of ovarian cysts. Saudi Med J. 2015 Jul;36(7):834-8. DOI: 10.15537/smj.2015.7.11690
[31] Bdeiwi H, Sultan H, Mezketli Z, Jouma Al-Hejazi T, Trissi M, Kellawi K, Zayat R, Al-Hammod A. An unusual site for hydatid cyst on ovary misdiagnosed as an ovarian cyst: a case report. Ann Med Surg (Lond). 2023 Jul;85(7):3735-3738. DOI: 10.1097/MS9.0000000000001004




