[Die Meatus-Nasi-Plastik: ein Beitrag zur plastischen Rekonstruktion der Nasenklappe beim Midfacial Degloving]
Kai J. Lorenz 1Heinz Maier 1
Frank Wilde 2
1 Clinic for Otorhinolaryngology, Head and Neck Surgery, Federal Armed Forces Hospital, Ulm, Germany
2 Clinic for Oral, Maxillary and Plastic Facial Surgery, Federal Armed Forces Hospital, Ulm, Germany
Zusammenfassung
Das Midfacial Degloving hat sich als übersichtlicher Zugang zum Mittelgesicht, der Nasenpyramide, den Sinus maxillares et ethmoidales, der Orbita sowie der vorderen Schädelbasis bewährt. Indikationen für diesen Zugang sind vor allem Tumorresektionen im Bereich des Mittelgesichts, des Septums, der Kieferhöhlen, der Nasennebenhöhlen bis zur Keilbeinhöhle sowie des Clivus. Außerdem ermöglicht dieser Zugang die Exposition der knöchernen Strukturen des Mittelgesichts bei ausgedehnten Frakturen.
Grundsätzlich kombiniert dieser Zugang eine Inzision im Vestibulum oris sowie zirkuläre Inzisionen im Bereich des Vestibulum nasi zum Auslösen der Nasenpyramide.
Nach Entfernen der fazialen Kieferhöhlenwand gelingt dann die weite Exposition des Operationsgebietes.
Als nachteilig hat sich bei diesem Zugangsweg die schwierige Rekonstruktion der Nasenklappenregion erwiesen, die häufig zu narbigen Stenosen mit Nasenatmungsbehinderungen führt. Ebenso werden Wundheilungsstörungen und Radioosteonekrosen im Bereich der lateralen freien Kante der Apertura piriformis nach Reimplantation der facialen Kieferhöhlenwand beschrieben, da in diesem Bereich bei konventioneller Technik keine ausreichende Weichteildeckung möglich ist.
Wir beschreiben einen kranial und kaudal gestielten Weichteillappen im Bereich der Nasenklappe, der die Rekonstruktion des Vestibulum nasi ebenso wie eine ausreichende Weichteildeckung der Apertura piriformis ermöglicht.
Schlüsselwörter
Midfacial Degloving, Naseneingangsstenose, Nasennebenhöhlentumore
Introduction
Midfacial degloving is a proven surgical technique for accessing deeper areas of the midface, whose soft tissue coverage, a large skin flap, is cranially transposed. This technique was first described by Portmann in 1927, but the modern technique is based on the work of Casson and dates from 1974 [6]. In 1979, Conley and Price published first results in the treatment of malignant paranasal sinus processes [7]. In German-speaking countries, the midfacial degloving approach was primarily introduced by the work of Berghaus [2], [3]. This method of access is basically a combination of rhinoplasty and sublabial-transfacial access via an oral vestibule incision. Advantages of the midfacial degloving approach are a good overview that permits extensive exploration of the entire paranasal sinus system, the anterior skull base, and the septum [1], [3], [4], [5], [8], [9], [11], [13], [14], [16], [17], [19], [20], [24], [25]. If required, it also allows for a bilateral approach and a working direction parallel to the skull base and the lamina papyracea [3], [7]. Finally, this method of access does not leave any visible scars on the patient’s face [6], [7]. The midfacial degloving approach is thus a good alternative to the usual methods of access to the midfacial skeleton and the anterior skull base such as the transmaxillary approach according to Denker, transpalatinal techniques, and transfacial incisions such as a lateral rhinotomy with transposition of the facial nerve and the mandible.
Indications for midfacial degloving include malignant tumours of the paranasal sinuses and the anterior skull base, the septum and the nasal cavity, as well as inverted papilloma and, with restrictions, tumours of the nasopharynx. Midfacial degloving is also used as a method of access in midfacial traumatology [1], [4], [7], [8], [16], [20]. In combination with a coronal incision, the midfacial degloving approach makes the exploration of the entire frontal facial skeleton possible.
Apart from the advantages, midfacial degloving also entails a few possible complications. These include sensory disturbance of the area innervated by the trigeminal nerve (V2) and nasolacrimal duct stenoses as well as postoperative large encrusting wound cavities [4], [6], [19]. These complications are not only associated with midfacial degloving, however, but with all surgical techniques that leave behind large wound cavities due to extensive resections. In addition, stenoses in the nasal valve area are possible, as well as osteonecroses in the area of the margin of the anterior nasal aperture not covered by soft tissue, especially when the facial wall of the maxillary sinus has been replanted in the course of osteoplastic work. The latter complications can be observed if insufficient attention was paid to adapting the incision edges in the reconstruction of the nasal vestibule. Osteonecroses are a possible complication when patients who have undergone midfacial degloving because of malignant tumours in the area of the paranasal sinuses receive postoperative radiation. In order to avoid these complications, we developed a soft tissue flap pedicled in the basal and cranial directions in the area of the nasal vestibule which allows coverage of the bone margin not covered by soft tissue and the reconstruction of the nasal vestibule.
Surgical technique
As described in the works of Berghaus, Conley and Price [2], [3], [7], the midfacial degloving approach is a combination of four types of incisions (Figure 1 [Fig. 1]):
Figure 1: Depiction of incisions used to prepare the meatus flap. Creation of 5–10 mm wide mucosal soft tissue flap pedicled in the cranial and caudal directions.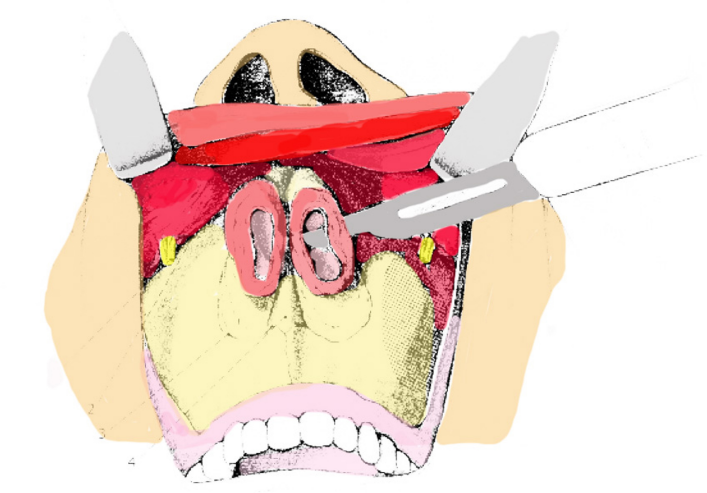
- Transfixion incision
- Bilateral intercartilaginous incisions
- Bilateral circumvestibular incisions
- Bilateral sublabial incision across the midline in the fold of the oral vestibule.
Next, the periosteum of the nasal skeleton is prepared. After connecting all incisions, the soft tissues of the midface including the alar cartilages can now be jointly elevated away from the upper lip, cheek and nose and moved upwards. In doing so, care must be taken not to injure the infraorbital nerve.
The next step is dissecting the soft tissue including the mucous membrane in the area of the margin of the anterior nasal aperture and of the lateral wall of the nasal cavity by preparing the border of the inferior nasal concha. If necessary, the bony border of the inferior concha can be separated from the lateral septum with a chisel. The preparation of the meatus flap begins with the removal by scalpel of an approximately 0.5 cm wide strip of mucosal soft tissue parallel to the margin of the anterior nasal aperture from the mucosal parts of the lateral nasal cavity wall (Figure 2 [Fig. 2]). It must be ensured that this strip of mucous membrane remains pedicled both in the cranial and the caudal directions; this is a major precondition for the blood supply of this meatus flap. The meatus flap is transposed medially towards the septum and fixed with a small purse-string suture if necessary. An osteotomy can now be performed in the area of the facial wall of the maxillary sinus as usual. If required by the extension of the process, this osteotomy is combined with an osteotomy in the area of the lateral wall of the nasal cavity, so that sufficient exploration of the maxillary sinus, the paranasal sinus system, the nasal cavity and the entire septum is possible.
Figure 2a and b: Preparation of meatus flap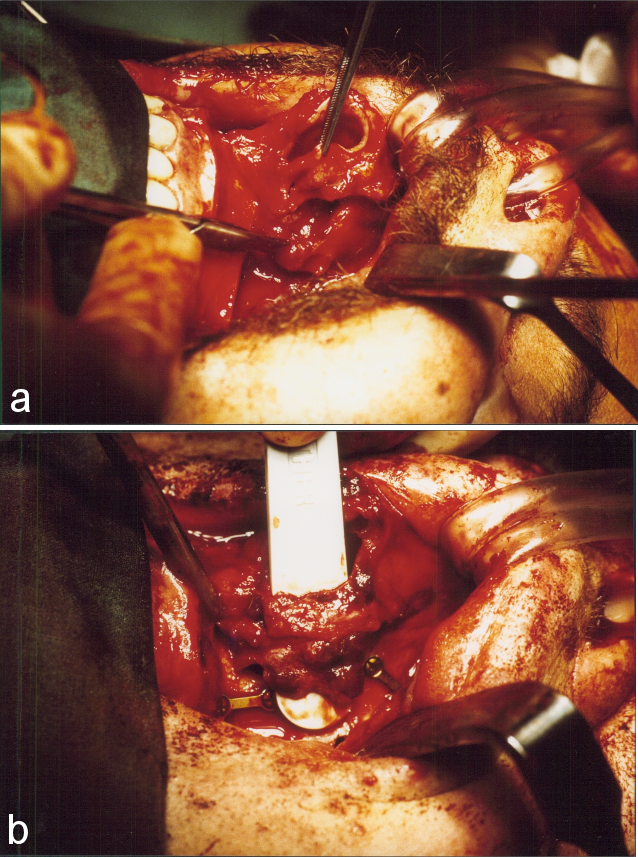
After resection surgery, the nasal vestibule is reconstructed with the meatus flap described above. For this purpose, three to four small holes are drilled into the area of the anterior nasal aperture and the previously removed maxillary sinus front wall. The bone flap is then replanted either with absorbable sutures or with mini plate fixation (Figure 3 [Fig. 3]). The mucosal flap can now be securely fixed to the boreholes at the anterior nasal aperture by absorbable sutures (Figure 4 [Fig. 4]). This ensures soft tissue coverage of the bone margin. After the soft tissue cover is put back in place, the nasal valve can safely be reconstructed on the soft tissue already fixed in the area of the nasal vestibule. In this way, vestibular stenosis can usually be prevented (Figure 5 [Fig. 5]).
Figure 3: Refixed facial wall of the maxillary sinus with boreholes in the area of the anterior nasal aperture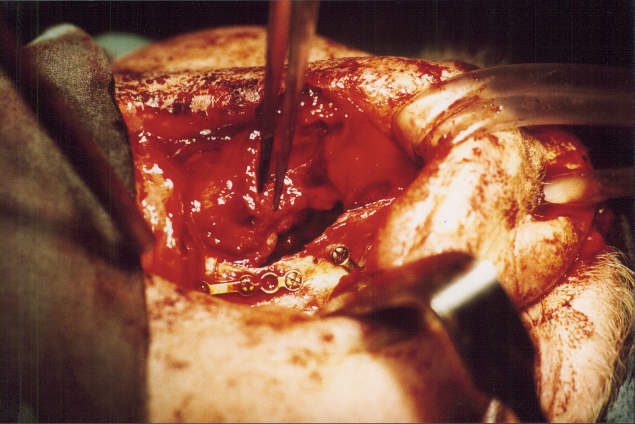
Figure 4: Fixation of meatus flap on the anterior nasal aperture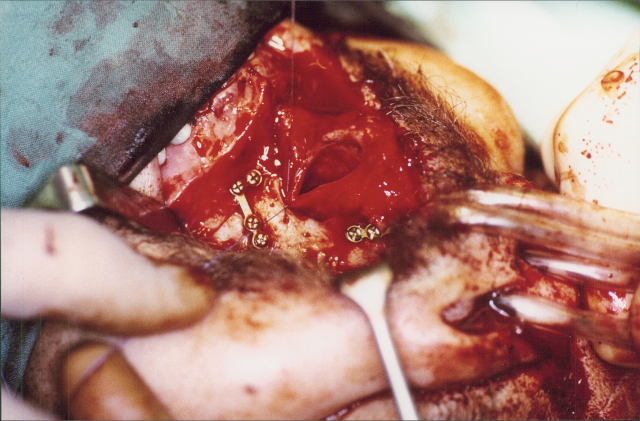
Figure 5: Postoperative result approximately 8 weeks after surgery with meatus plasty
Results
Midfacial degloving is a technique we have been using for 23 years now. A total of 72 patients have undergone this type of surgery. We have been performing meatus plasty in the manner described above for 19 years now, in which time 57 patients have undergone this surgery. Indications have included malignant tumours of the nasal septum, the nasal conchae, the maxillary sinuses, the ethmoid bone, and inverted papilloma that could not be safely removed with an endoscope (Table 1 [Tab. 1]). In the group of patients who underwent conventional surgery, we observed 5 cases of vestibular stenosis (Figure 6 [Fig. 6]) and 2 cases of osteonecrosis in the area of the replanted maxillary sinus bone flap after radiation. In the group of patients who underwent meatus plasty, we observed one case of vestibular stenosis and no case of osteoradionecrosis after radiation (Table 1 [Tab. 1]). This technique did not significantly prolong surgery time. Postoperative swelling that abated within one week was found in 34 patients. There were three cases of secondary haemorrhaging that was stopped by a tamponade. One patient developed a vestibulonasal fistula that had to be treated surgically.
Table 1: Patient characteristics and postoperative complications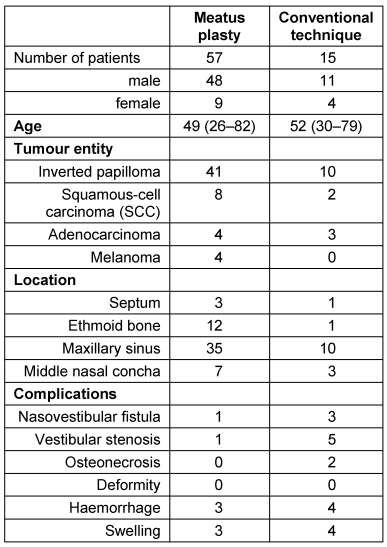
Figure 6: Postoperative result for patient without meatus plasty with vestibular stenosis
Discussion
Since its description by Casson and his staff in 1974 [6] and by Conley and Price [7] in 1979, midfacial degloving has proven to be a successful method of exploring the midface and the paranasal sinus system underneath. In particular because of the good aesthetic postoperative results without visible external scars, this method of access can also be used for benign tumours and especially with young patients. In particular, disfigurations due to scarring and functional damage due to a distortion of the nasal alae or ectropion with epiphora can be avoided. In addition to extended paranasal sinus surgery, especially in the case of inverted papilloma, this method of access has proven successful for space occupying lesions on the septum, in trauma treatment of the entire midfacial complex, and in the resection of juvenile nasopharyngeal angiofibromas [1], [4], [5], [9], [13], [16], [18], [21], [22], [23], [24], [25]. Further indications include tumours of the upper jaw and alveolar cysts [15], [26], [28], [29]. When this approach is combined with endoscopic techniques, more indications can be added to the list [10], [12], [27].
One problem with this method of access is the difficult reconstruction in the nasal valve area, which entails a considerable risk of vestibular stenosis (Figure 6 [Fig. 6]) and possibly insufficient soft tissue coverage, particularly on the margin of the replanted facial wall of the maxillary sinus. Our modification along the lines of a meatus plasty makes it possible to safely and easily avoid these complications to a large extent, because it ensures that the bone margin of the replanted bone flap is covered with soft tissue. By fixing the mucosal flap to the bone, we create a kind of buttress sufficiently to the front towards the nasal valve which allows for smooth and easy repositioning and fixation of the frontal nasal valve with a reduced risk of vestibular stenosis. The meatus plasty technique presented here is thus a fast, simple and safe alternative to nasal valve reconstruction during midfacial degloving. It is especially useful for tumours of the lateral nasal septum which necessitate a resection of the inferior nasal concha and of parts of the medial wall of the maxillary sinus. If tumours are too close to the nasal vestibule, the remaining soft tissue may be insufficient for a meatus flap. In all other cases, problem-free preparation is possible. In order to ensure an adequate supply of blood, the flap needs to remain pedicled in the cranial and caudal directions. Otherwise, scarring may lead to constriction of the nasal valve.
In addition, we temporarily fix the flap onto the septum with two sutures, so as not to endanger the 1–2 cm wide flap during surgery and in order to maintain a good overview of the surgical site. This technique is particularly suitable if there are pathological findings that require a resection of the inferior nasal concha or the lateral nasal septum. The complication rate of this surgery is very low. There has been no case with major complications. The oronasal fistula involving the oral vestibule which we observed in two cases is very rare and can usually be prevented by means of a careful stitching technique.
Notes
Competing interests
The authors declare that they have no competing interests.
References
[1] Baumann A, Ewers R. Midfacial degloving: an alternative approach for traumatic corrections in the midface. Int J Oral Maxillofac Surg. 2001 Aug;30(4):272-7. DOI: 10.1054/ijom.2001.0106[2] Berghaus A. Midfacial degloving. HNO. 1990 Jan;38(1):7-11.
[3] Berghaus A, Jovanovic S. Technique and indications of extended sublabial rhinotomy ("midfacial degloving"). Rhinology. 1991 Jun;29(2):105-10.
[4] Browne JD. The midfacial degloving procedure for nasal, sinus, and nasopharyngeal tumors. Otolaryngol Clin North Am. 2001 Dec;34(6):1095-104, viii. DOI: 10.1016/S0030-6665(05)70368-6
[5] Buchwald C, Bonding P, Kirkby B, Fallentin E. Modified midfacial degloving. A practical approach to extensive bilateral benign tumours of the nasal cavity and paranasal sinuses. Rhinology. 1995 Mar;33(1):39-42.
[6] Casson PR, Bonanno PC, Converse JM. The midface degloving procedure. Plast Reconstr Surg. 1974 Jan;53(1):102-3. DOI: 10.1097/00006534-197401000-00026
[7] Conley J, Price JC. Sublabial approach to the nasal and nasopharyngeal cavities. Am J Surg. 1979 Oct;138(4):615-8. DOI: 10.1016/0002-9610(79)90431-8
[8] deFries HO, Deeb ZE, Hudkins CP. A transfacial approach to the nasal-paranasal cavities and anterior skull base. Arch Otolaryngol Head Neck Surg. 1988 Jul;114(7):766-9. DOI: 10.1001/archotol.1988.01860190070026
[9] Draf W, Berghaus A. Tumoren und Pseudotumoren ("tumorähnliche Läsionen") der frontalen Schädelbasis, ausgehend von der Nase, den Nasennebenhöhlen und dem Nasenrachenraum (einschliesslich der operativen Zugänge). Rhinochirurgisches Referat [Tumors and pseudotumors ("tumor-like lesions") of the frontal cranial base, originating in the nose, the paranasal sinuses and the nasopharynx (including surgical approach)]. Eur Arch Otorhinolaryngol Suppl. 1993;1:105-86.
[10] El-Banhawy OA, Shehab El-Dien Ael-H, Amer T. Endoscopic-assisted midfacial degloving approach for type III juvenile angiofibroma. Int J Pediatr Otorhinolaryngol. 2004 Jan;68(1):21-8. DOI: 10.1016/j.ijporl.2003.09.013
[11] Ferreira LM, Rios AS, Gomes EF, Azevedo JF, Araújo Rde P, Moraes RB. Midfacial degloving--access to nasal cavity and paranasal sinuses lesions. Braz J Otorhinolaryngol. 2006 Mar-Apr;72(2):158-62.
[12] Ikeda K, Suzuki H, Oshima T, Nakatsuka S, Takasaka T. Midfacial degloving approach facilitated by endoscope to the sinonasal malignancy. Auris Nasus Larynx. 1998 Sep;25(3):289-93. DOI: 10.1016/S0385-8146(97)10040-2
[13] Jeon SY, Jeong JH, Kim HS, Ahn SK, Kim JP. Hemifacial degloving approach for medial maxillectomy: a modification of midfacial degloving approach. Laryngoscope. 2003 Apr;113(4):754-6. DOI: 10.1097/00005537-200304000-00032
[14] Kainuma K, Netsu K, Asamura K, Hayashi K, Takumi Y, Ota H, Usami S. Chondrosarcoma of the nasal septum: A case report. Auris Nasus Larynx. 2009 Oct;36(5):601-5. DOI: 10.1016/j.anl.2008.12.006
[15] Kitagawa Y, Baur D, King S, Helman JI. The role of midfacial degloving approach for maxillary cysts and tumors. J Oral Maxillofac Surg. 2003 Dec;61(12):1418-22. DOI: 10.1016/j.joms.2002.09.001
[16] Lafond G. Modification of the sublabial approach to midface, nasopharynx, and postnasal tumors. J Otolaryngol. 1985 Jun;14(3):183-6.
[17] Lenarz T, Keiner S. Midfacial Degloving: ein alternativer Zugangsweg zur Frontobasis, der Nasenhaupt- und den Nasennebenhöhlen [Midfacial degloving: an alternative approach to the frontobasal area, the nasal cavity and the paranasal sinuses]. Laryngorhinootologie. 1992 Aug;71(8):381-7. DOI: 10.1055/s-2007-997320
[18] Lindemann J, Leiacker R, Sikora T, Rettinger G, Keck T. Impact of unilateral sinus surgery with resection of the turbinates by means of midfacial degloving on nasal air conditioning. Laryngoscope. 2002 Nov;112(11):2062-6. DOI: 10.1097/00005537-200211000-00029
[19] Maniglia AJ. Indications and techniques of midfacial degloving. A 15-year experience. Arch Otolaryngol Head Neck Surg. 1986 Jul;112(7):750-2. DOI: 10.1001/archotol.1986.03780070062013
[20] Maniglia AJ, Phillips DA. Midfacial degloving for the management of nasal, sinus, and skull-base neoplasms. Otolaryngol Clin North Am. 1995 Dec;28(6):1127-43.
[21] Midilli R, Karci B, Akyildiz S. Juvenile nasopharyngeal angiofibroma: analysis of 42 cases and important aspects of endoscopic approach. Int J Pediatr Otorhinolaryngol. 2009 Mar;73(3):401-8. DOI: 10.1016/j.ijporl.2008.11.005
[22] Osguthorpe JD, Patel S. Craniofacial approaches to tumors of the anterior skull base. Otolaryngol Clin North Am. 2001 Dec;34(6):1123-42, ix. DOI: 10.1016/S0030-6665(05)70370-4
[23] Papadogeorgakis N, Petsinis V, Eleftheriades E, Dimtsas S, Protopappa D, Alexandridis C. Large olfactory neuroblastoma (esthesioneuroblastoma) surgically treated with an Altemir technique modification: a case report. Oral Maxillofac Surg. 2009 Sep;13(3):171-5. DOI: 10.1007/s10006-009-0160-x
[24] Plinkert PK, Zenner HP. Transfazialer Zugang, kraniofaziale Resektion und Midfacial Degloving bei der Chirurgie bösartiger Tumoren der vorderen Schädelbasis und der angrenzenden Nasennebenhöhlen [Transfacial approach, craniofacial resection and midfacial degloving in surgery of malignant tumors of the anterior cranial base and adjacent paranasal sinuses]. HNO. 1996 Apr;44(4):192-200.
[25] Price JC. The midfacial degloving approach to the central skull-base. Ear Nose Throat J. 1986 Apr;65(4):174-80.
[26] Westhofen M, Mautsch W, Blaum M. Oberkiefertotalresektion via Midfacial Degloving [How I do it - total maxillectomy via midfacial degloving]. Laryngorhinootologie. 2001 Sep;80(9):542-5. DOI: 10.1055/s-2001-17093
[27] Wigand ME, Iro H, Bozzato A. Transcranial combined neurorhinosurgical approach to the paranasal sinuses for anterior skull base malignancies. Skull Base. 2009 Mar;19(2):151-8. DOI: 10.1055/s-0028-1096200
[28] Yang SJ, Choi JW, Chung YS, Ahn KM, Hong JP, Lee TJ, Koh KS. Midfacial degloving approach for resectioning and reconstruction of extensive maxillary fibrous dysplasia. J Craniofac Surg. 2012 Nov;23(6):1658-61. DOI: 10.1097/SCS.0b013e31826460fd
[29] Zaghloul AS, Nouh MA, Fatah HA. Midfacial degloving approach for malignant maxillary tumors. J Egypt Natl Canc Inst. 2004 Jun;16(2):69-75.




