Recurrent spine surgery patients in hospital administrative database
M. Sami Walid 1Nadezhda Zaytseva 2
Lyudmila Porubaiko 2
Moataz Abbara 3
1 Medical Center of Central Georgia, Macon, USA
2 Kuban State Medical University, Krasnodar, Russia
3 Alwatani Hospital, Homs, Syria
Abstract
Introduction: Hospital patient databases are typically used by administrative staff to estimate loss-profit ratios and to help with the allocation of hospital resources. These databases can also be very useful in following rehospitalization. This paper studies the recurrence of spine surgery patients in our hospital population based on administrative data analysis.
Methods: Hospital data on 4,958 spine surgery patients operated between 2002 and 2009 were retrospectively reviewed. After sorting the cohort per ascending discharge date, the patient official name, consisting of first, middle and last names, was used as the variable determining duplicate cases in the SPSS statistical program, designating the first case in each group as primary. Yearly recurrence rate and change in procedure distribution were studied. In addition, hospital charges and length of stay were compared using the Wilcoxon-Mann-Whitney test.
Results: Of 4,958 spine surgery patients 364 (7.3%) were categorized as duplicate cases by SPSS. The number of primary cases from which duplicate cases emerged was 327 meaning that some patients had more than two spine surgeries.
Among primary patients (N=327) the percentage of excision of intervertebral disk procedures was 33.3% and decreased to 15.1% in recurrent admissions of the same patients (N=364). This decrease was compensated by an increase in lumbar fusion procedures. On the other hand, the rate of cervical fusion remained the same.
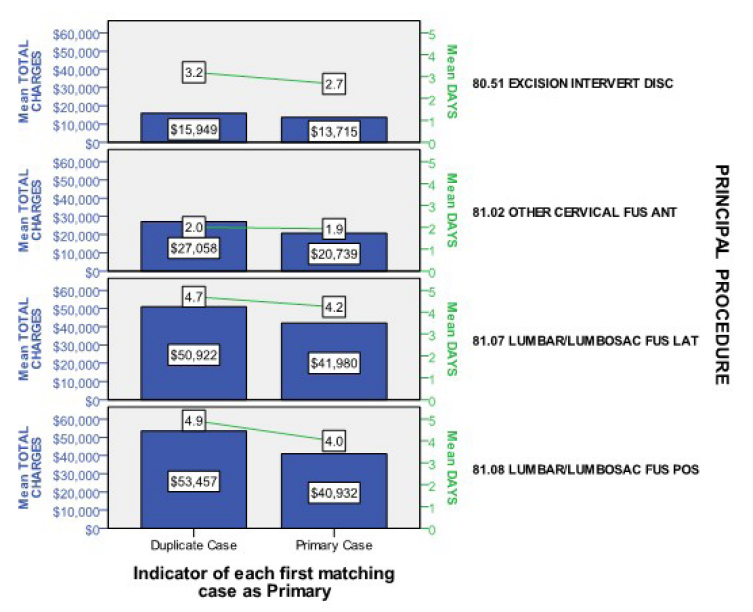
The difference in hospital charges between primary and duplicate patients was $2,234 for diskectomy, $6,319 for anterior cervical fusion, $8,942 for lumbar fusion – lateral technique, and $12,525 for lumbar fusion – posterior technique. Recurrent patients also stayed longer in hospital, up to 0.9 day in lumbar fusion – posterior technique patients.
Conclusion: Spine surgery is associated with an increasing possibility of additional spine surgery with rising invasiveness and cost.
Keywords
recurrent spine surgery, hospital charges, cost, length of stay
Introduction
In industrial nations with advanced healthcare systems and improved longevity degenerative spine disorders are steadily increasing parallel to the aging of the population. Thanks to the sharp developments in spine instrumentation, a higher percentage of patients with back problems are now being effectively treated using fusion techniques, especially in the United States [1].
Hospital patient databases are typically used by administrative staff to estimate loss-profit ratios and to help with the allocation of hospital resources. These databases can also be very useful in following rehospitalization. This paper studies the recurrence of spine surgery patients in our hospital population based on administrative data analysis.
Methods
A continuous cohort of 6,147 spine surgery patients operated at the Medical Center of Central Georgia between October 2002 and September 2009 were retrieved from the administrative data of the hospital. The Medical Center of Central Georgia MCCG is a 637-bed, full-service, acute care hospital, the second largest in the state, that serves an estimated population of 750,000 residents in central Georgia (Emergency Medical Services Region EMS-5). Eight neurosurgeons and forty three orthopedic surgeons (2008) practice in independent groups to provide spine care for their patients in EMS-5. Surgeons admit elective cases to the hospital to be operated and discharged at their own liability.
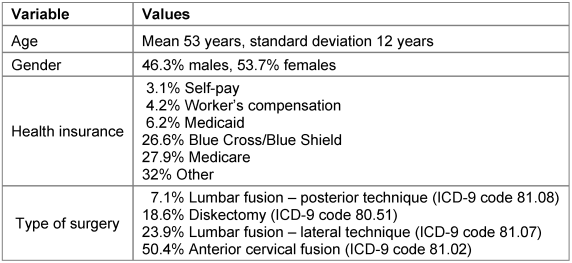
Preliminary analysis of the patient cohort showed that the top five most common procedures were anterior cervical decompression and fusion (ICD-9 code 81.02), lumbar decompression and fusion – lateral transverse process technique (ICD-9 code 81.07), lumbar diskectomy (ICD-9 code 80.51), spinal canal exploration (ICD-9 code 03.09) and lumbar decompression and fusion – posterior technique (ICD-9 code 81.08). These procedures made 89% (5,469) of the total cohort. Posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF) were coded under the posterior technique (ICD-9 81.08). Excluding spinal canal exploration, being a nonspecific procedure that may relate to an oncologic or traumatic case, 4,958 (81%) patients remained and were used as the study cohort (Table 1 [Tab. 1]).
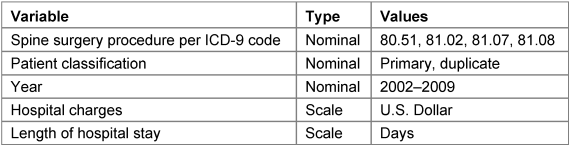
After sorting the cohort per ascending discharge date, the patient official name, consisting of first, middle and last names, was used as the variable determining duplicate cases in the SPSS statistical program, designating the first case in each group as primary (Table 2 [Tab. 2]). Our goal was to study the recurrence of spine surgery patients due mainly to degenerative disease. Yearly recurrence rate and changes in procedure distribution were analyzed. Hospital charges and length of stay were compared using the Wilcoxon-Mann-Whitney test.
Study limitations
The study was based on an eight year continuous cohort of spine surgery patients some of which may have underwent spine surgery in the past and were therefore not de novo patients. In addition, some patients might have changed healthcare provider due to travel or personal preference and received additional care or intervention at another place.
Results
Recurrence rate
Of 4,958 spine surgery patients 364 (7.3%) were categorized as duplicate cases by SPSS. The number of primary cases from which duplicate cases emerged was 327 meaning that some patients had more than two spine surgeries. The percentage of recurrent spine surgery patients increased eight-fold from 2002 to 2009. The percentages were as follows: 1.45% (2002), 2.66% (2003), 5.25% (2004), 6.05% (2005), 7.92% (2006), 8.05% (2007), 8.66% (2008), and 12.24% (2009).
Shift in procedure type in recurrent patients
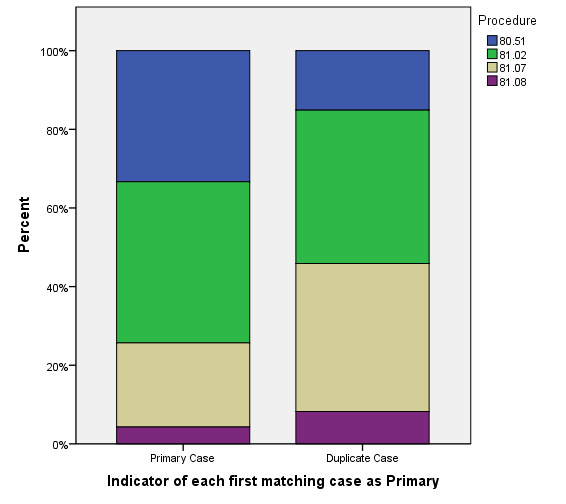
Among primary patients (N=327) the percentage of excision of intervertebral disk procedures was 33.3% (Figure 1 [Fig. 1]) and decreased to 15.1% in recurrent admissions of the same patients (N=364). This decrease was compensated by an increase in lumbar fusion procedures (21.4% vs. 37.6% for lateral fusion in primary and duplicate patients respectively and 4.3% vs. 8.2% for posterior fusions in primary and duplicate patients respectively). On the other hand, the rate of cervical fusion remained the same (41.0% vs. 39.0% in primary and duplicate patients respectively).
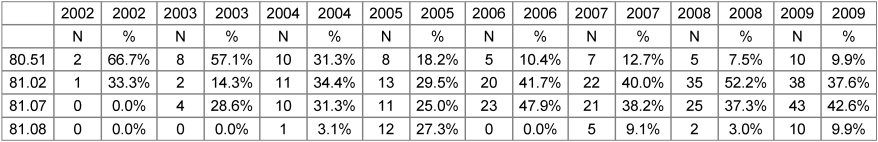
From 2002 to 2009, the percentage of recurrent diskectomy patients among all duplicate patients decreased seven-fold from 66.7% to 9.9%; anterior cervical fusion patients remained the same (33.3% in 2002 vs. 37.6% in 2009); and lumbar fusion – lateral technique and posterior technique increased from 0% to 42.6% and 9.9% respectively (Table 3 [Tab. 3]).
Cost of recurrent spine surgery
Comparing the average hospital charges of recurrent spine procedures with primary procedures a significant difference was noted. The difference in hospital charges was $2,234 for diskectomy, $6,319 for anterior cervical fusion, $8,942 for lumbar fusion – lateral technique, and $12,525 for lumbar fusion – posterior technique. Recurrent patients also stayed longer in hospital, up to 0.9 day in lumbar fusion – posterior technique patients (Figure 2 [Fig. 2]).
Discussion
Our study demonstrates the usefulness of administrative data in tracking recurrent spine surgery patients. The study demonstrates that recurrent spine surgery patients accumulate from year to year with a shift of procedure type to fusion and concomitant increase in consumption of hospital resources.
Several physiological, mechanical, pathological, psychological and external factors may explain the phenomenon of recurrent spine surgery. Aging and progressive degenerative spine disease are continuous synchronous processes that affect all people; however not all people need spine surgery, not to say repeated spine surgery. Physiologically, there are individual factors inherent to every person’s organism that may increase susceptibility for degenerative spine disorders, i.e. genetic traits and constitutional characteristics. The degenerative process may also be accelerated by external factors such as the category of occupation and the variety of hobbies practiced as well as the number of motor vehicle accidents suffered. Most reoperations appear to happen in the lower vertebral levels [2], probably because the neck is subjected to less torque force and weight burden than the lumbar spine. However, the risk of distant surgical intervention on upper levels may increase as well [3], [4], [5], [6], [7] if the spinal axis and center of gravity is significantly disturbed [5]. From a psychological point of view, patients with recurring spine pain and chronic opioid (ab)use, having felt subjective relief from earlier operative intervention and postoperative analgesia, may more willingly seek surgical treatment compared with de novo patients [6]. On the other hand, patients may require additional spine surgery as result of a diffuse organic disease afflicting the spine (e.g. ankylosing spondylitis) or the whole skeleton (e.g. osteoporosis).
In the United States, a 220% increase in the rate of lumbar spine fusion surgery from 1990 to 2001 was recorded [7]. The availability of healthcare providers and healthcare insurance coverage coupled with high patient expectations seems to facilitate patient access to expensive spine surgery. In this context, one may ask the following questions:
- If a patients can get a service and a third party will pay for it, will the patient be more likely to request the service? [8], [9]
- If a surgeon provides a service for a fee, will the surgeon be more likely to provide the service if requested? [10]
This double bias seems to have synergistically contributed to the dramatic increase in spine surgery rate and healthcare expenditures in general [11]. Bias however, as Cain and Detsky stated in their 2008 JAMA article, “is not a crime, is not necessarily intentional, and is not a sign of lack of integrity; rather, it is a natural human phenomenon” [12].
The take-away message from this paper is that a significant percentage of patients are predisposed to multiple spine interventions of increasing invasiveness. Insofar as this study provides a basis for contemplation, considering reoperation in the outcome analysis of spine surgery is essential to understand the clinical dynamics of spine patients and better prognosticate their long-term course.
Notes
Competing interests
The authors declare that they have no competing interests.
References
[1] Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine (Phila Pa 1976). 1994;19(11):1201-6.[2] Walid MS, Zaytseva N. History of spine surgery in older obese patients. GMS Ger Med Sci. 2011;9:Doc05. DOI: 10.3205/000128.
[3] Lee JK, Amorosa L, Cho SK, Weidenbaum M, Kim Y. Recurrent lumbar disk herniation. J Am Acad Orthop Surg. 2010;18(6):327-37.
[4] Wang S, Xia Q, Passias P, Li W, Wood K, Li G. How does lumbar degenerative disc disease affect the disc deformation at the cephalic levels in vivo? Spine (Phila Pa 1976). 2011;36(9):E574-81. DOI: 10.1097/BRS.0b013e3181f79e93
[5] Matsunaga S, Sakou T, Nakanisi K. Analysis of the cervical spine alignment following laminoplasty and laminectomy. Spinal Cord. 1999;37(1):20-4. DOI: 10.1038/sj.sc.3100749
[6] Walid MS, Robinson JS 3rd, Abbara M, Tolaymat A, Robinson JS Jr. De novo spine surgery as a predictor of additional spine surgery at the same or distant spine regions. GMS Ger Med Sci. 2011;9:Doc10. DOI: 10.3205/000133.
[7] Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005;30(12):1441-5; discussion 1446-7.
[8] Brett AS, McCullough LB. When patients request specific interventions: Defining the limits of the physician's obligation. N Engl J Med. 1986;315(21):1347-51. DOI: 10.1056/NEJM198611203152109
[9] Brett AS, McCullough LB. Addressing requests by patients for nonbeneficial interventions. JAMA. 2012;307(2):149-50. DOI: 10.1001/jama.2011.1999
[10] Hollenbeck BK, Nallamothu BK. Financial incentives and the art of payment reform. JAMA. 2011;306(18):2028-30. DOI: 10.1001/jama.2011.1630
[11] Emanuel EJ, Fuchs VR. The perfect storm of overutilization. JAMA. 2008;299(23):2789-91. DOI: 10.1001/jama.299.23.2789
[12] Cain DM, Detsky AS. Everyone's a little bit biased (even physicians). JAMA. 2008;299(24):2893-5. DOI: 10.1001/jama.299.24.2893