Progressive fluid removal can avoid electrolyte disorders in severely burned patients
Thomas Namdar 1Peter Leonard Stollwerck 1
Felix Hagen Stang 1
Georgios Kolios 2
Thomas Lange 1
Peter Mailänder 1
Frank Siemers 1
1 Department of Plastic Surgery, Hand Surgery, Burn Unit, University Hospital Schleswig-Holstein Campus Lübeck, Germany
2 Agaplesion Diakonieklinikum Hamburg, Germany
Abstract
Introduction: Extensive burn injury has systemic consequences due to capillary leak. After restoration of cellular integrity, infused fluid volume has to be removed partially. This can provoke electrolyte disorders.
Purpose: We investigated the effect of progressive fluid removal on serum sodium level.
Method: Retrospective study. Patients admitted to a burn unit were analyzed and separated in two groups without (Group A) or with (Group B) prolonged hypernatremia. Daily infusion-diuresis-ratio (IDR) was analyzed.
Results: Fourty (12 female; 28 male) patients with a mean age of 47±19 years, a total burn surface area (TBSA) of 26±12%, and a mean abbreviated burned severity index (ABSI) score of 7.3±2 were included. In Group A 25 patients with a mean age of 47±18 years, a mean TBSA of 23±11%, and a mean ABSI score of 6.9±2.1 were summarized. In Group B 15 patients with a mean age of 47±22 years, a mean TBSA of 30±13%, and a mean ABSI score of 8.1±1.7 were included. Hypernatremia occurred on day 5±1.4. There was no significant difference between both groups for fluid resuscitation amount within the first 24 hours. Statistical analysis of the first 7 days after burn injury showed a significantly higher percentage of removed fluid in Group B for day 3, day 4, day 5, day 6 and day 7.
Conclusions: Amount and velocity of fluid removal regimen after burn injury can provoke electrolyte disorders. Serum sodium concentration can be used to calculate need of fluid resuscitation for fluid maintenance. There is a need of an established fluid removal strategy.
Keywords
burn injury, critical care, diuresis
Introduction
The skin – as the largest human organ – protects against infection and radiation, fluid and electrolyte loss. On the other hand the skin provides thermal regulation [1]. Thermal injury is a dynamic process that peaks at about 3 days after trauma and can affect the skin partially or completely [2], [3]. In case of long term or extremely hot thermal trauma injured structures may extend to subcutaneous tissue. In severely burned patients microvascular integrity is lost, and a plasma-like fluid leaks into the interstitial space. The time after injury at which capillary integrity is restored varies individually [4]. During this period plasma volume must be maintained to ensure tissue oxygen delivery.
Several established formulas describe kind and amount of fluid resuscitation during burn shock. The Parkland formula uses crystalloid alone and is frequently applied [5]. After recovering of cellular integrity the circulating fluid volume has to be normalized. Hereby extensive water and electrolyte shifts can provoke electrolyte disorders and systemic dehydration [6].
Partial thickness burns usually blister and protection against fluid loss is lost. In relation to the total burn surface area (TBSA) a systemic relevant fluid loss can occur. The transdermal fluid loss was calculated with 40 ml/%-TBSA/day [7]. Through this study, we want to elucidate the effect of progressive fluid removal regimen on serum sodium concentration in severely burned patients.
Materials and methods
Patients admitted to our specialized burn unit were analyzed retrospectively for the incidence and duration of hypernatremia (>146 mmol/l) as a sign for dehydration. Patient’s characteristics (age, sex, TBSA, abbreviated burned severity index (ABSI)) and continuous infusion-diuresis-ratio (IDR) were registered. Infusion volume summarizes saline and colloid infusion, as well as enteral nutrition. Diuresis was measured by permanent urine catheter. In a second step IDR after burn shock was put in relation to daily IDR or corrected by transdermal fluid loss (40 ml/%-TBSA). To investigate a relationship between percentage of removed volume and incidence of hypernatremia two subgroups have been build (Group A: without hypernatremia; Group B: with hypernatremia). We investigated IDR changes for the first 7 days after burn injury.
Statistics
Statistics were performed with SPSS 15.0 (SPSS Inc. Chicago, USA). To estimate significance between both groups Mann-Whitney-U-test or Chi-square-test were performed. Results are written in mean value ± standard deviation.
Results
In Group A 25 patients (7 female; 18 male) with a mean age of 47±18 years (minimum: 14 years; maximum: 73 years), a mean TBSA of 23±11% (minimum: 10%; maximum: 60%), and a mean ABSI score of 6.9±2.1 (minimum: 3; maximum: 11) were summarized. In Group B 15 patients (5 female; 10 male) with a mean age of 47±22 years (minimum: 17 years; maximum: 83 years), a mean TBSA of 30±13% (minimum: 12%; maximum: 70%), and a mean ABSI score of 8.1±1.7 (minimum: 5; maximum: 11) were included. Hypernatremia occurred on day 5±1.4 and persisted for 4.6±2.7 days (Table 1 [Tab. 1]).
Table 1: Patients characteristics written in mean ± standard deviation (sex, age [years], totally burned surface area (TBSA) [%], ABSI, burn shock fluid [ml/kg/%-TBSA]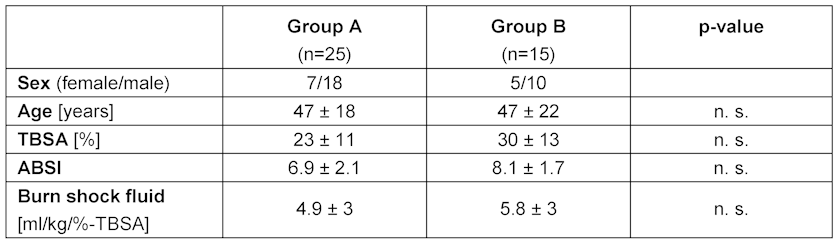
No significant difference in ABSI between both groups was found (p=0.078). There was no significant difference between both groups for fluid resuscitation amount within the first 24 hours (Group A vs. Group B 4.9±3 ml/kg/%-TBSA vs. 5.8±3 ml/kg/%-TBSA; p=0.32). In the analysis of daily IDR, we found – except for day 2 (p=0.06) – a significantly higher percentage of removed fluid in Group B (Table 2 [Tab. 2]). In the transdermal fluid loss corrected analysis a significantly higher percentage of removed volume was registered for day 4, day 5, day 6 and day 7 after burn injury (Table 3 [Tab. 3]). The 7 day course of non-corrected and corrected IDR-percentage is displayed in Figure 1 [Fig. 1].
Table 2: Percentual daily infusion-diuresis-ratio (IDR) divided in Group A (without) and Group B (with hypernatremia) and significance between both subgroups (n. s.: no significance)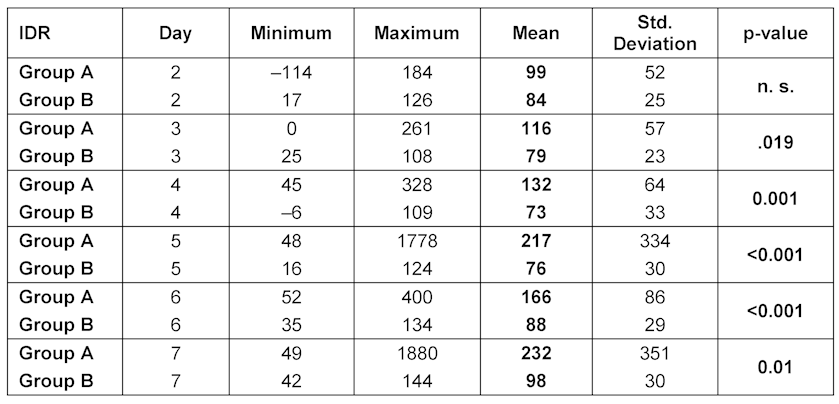
Table 3: Percentual daily infusion-diuresis-ratio (IDR) – corrected for transdermal fluid loss (40 ml/%-TBSA/day) divided in Group A (without) and Group B (with hypernatremia) and significance between both subgroups (n. s.: no significance)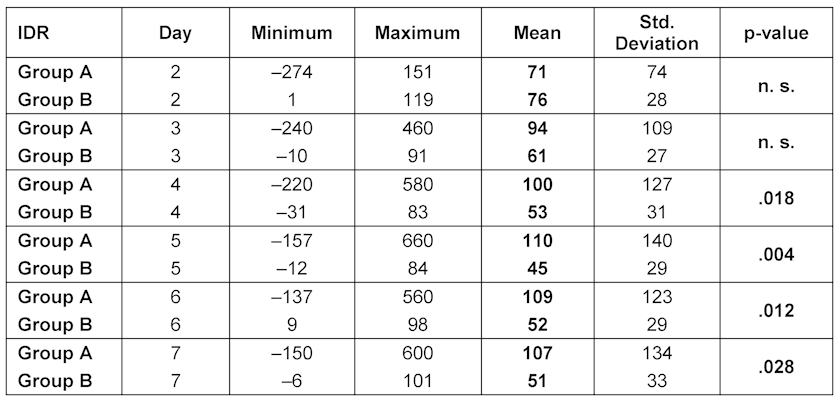
Figure 1: 7 day course of percentual fluid removal after burn shock resuscitation divided in Group A (without hypernatremia) and Group B (with hypernatremia) and corrected for transdermal fluid loss (40 ml/%-TBSA/day)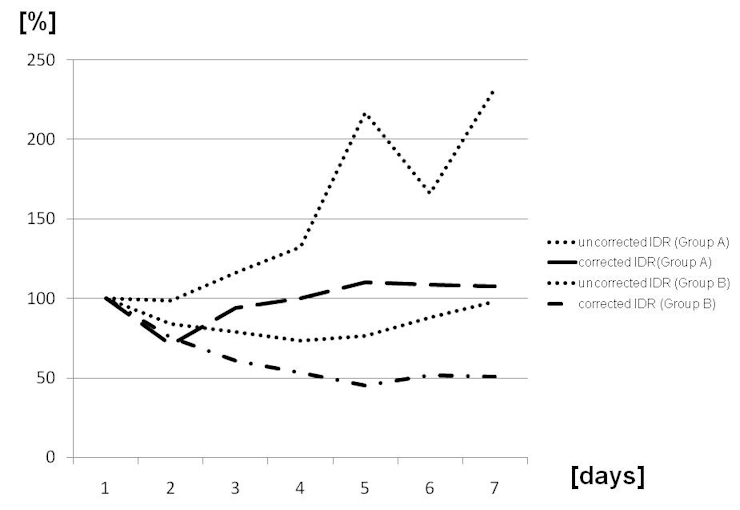
Discussion
There are several formulas to restore intravasal circulating fluid volume during burn shock. The Parkland formula – used in our burn unit – describes a need of ringer’s lactate infusate of 4 ml/kg/%-TBSA to replace interstitial fluid loss [8]. Fluid resuscitation within the first 24 hours is commonly monitored by measuring urinary output, haematocrit and mean arterial pressure. After – burn shock induced – capillary leak closure, soft tissue edema has to be reduced to advance patients conditions for skin grafting. After fluid removal resuscitation has only to maintain systemic fluid equilibrium. There is no evidenced data about amount (neither percentual, nor absolute) and velocity of fluid removal during this period.
To elucidate this question we compared 40 severely burned patients in regard to percentual alteration in daily IDR. Urinary output is an unreliable guide for individual need of fluid administration in the >48 hours post burn period, because respiratory water losses, osmotic diuresis secondary to accentuated glucose intolerance, high protein feeding, and derangements in hormone mechanisms contribute to increased fluid losses despite an adequate urine output [9]. In burned patients serum sodium concentration is the best guide for controlling fluid replacement >48 hours after burn injury and should be in normal range (135–145 mmol/l) [1]. Hypernatremia (>146 mmol/l) is a valid sign for systemic dehydration [10], [11], [12]. In severely burned patients hypernatremia is a frequently observed electrolyte disorder [4], [5], [13].
After burn injury there is a continuous transdermal fluid loss. Prior studies reported a wide range (25 to 80 ml/%-TBSA/day) of transdermal fluid loss [1], [14]. In our burn unit the transdermal fluid loss is calculated with 40 ml/%-TBSA/day. This fluid loss is terminated by complete reepithelization or after skin grafting surgery. In patients with a TBSA >10% transdermal fluid loss can have systemic effects. The fluid resuscitation during burn shock in our study was guided by Parkland formula [8], and fluid removal regimen was adjusted by measurement of hematocrit, central venous pressure, blood pressure, and urine output. Split skin grafting to deep dermal burn wounds was performed within 7 days after trauma.
We demonstrate in this study that patients with a hypernatremic state after burn shock showed a significantly higher percentual daily fluid removal within the first 7 days after trauma. This finding was registered in the non-corrected (day 3–day 7) and the transdermal-fluid-loss corrected analysis (day 4–day 7). The analysis without correction for transdermal fluid loss, showed no significantly difference in the amount of fluid regimen for day 1 and day 2 after burn injury. Same findings were calculated for the first 3 days after burn injury in the transdermal-fluid-loss corrected analysis.
Our findings show that a prolonged fluid removal regimen (>2 days) may provoke systemic electrolyte disorders and should be avoided. The amount of volume applied during resuscitation should be removed within 48 hours after capillary leak closure. In the following days a balanced daily IDR should be achieved. Therefore the individual amount of transdermal fluid loss has to be kept in mind. In patients with a prolonged fluid removal regimen a hypernatremic state was observed frequently. The transdermal fluid loss corrected analysis showed that in the hypernatremic subgroup the balanced fluid equilibrium was generated at about 50 percent of the maximum IDR (day 1). In the for transdermal fluid loss corrected normonatremic Group A the balanced fluid equilibrium was held on about 100% of the maximum IDR. There was neither a significant difference in the non-corrected, nor in the transdermal fluid loss corrected analysis of removed fluid volume within the first 2 days after burn injury between Group A and B.
We demonstrate that even in specialized high-volume burn centers the incidence of post-burn hypernatremia is not avoidable. Our findings enforce the assumption, that a post burn injury hypernatremic state can be provoked by prolonged fluid removal strategy. A negative daily IDR with a hypernatremic state indicates a relevant systemic dehydration [10], [11]. Hypernatremia should be immediately treated to avoid systemic dehydration and its neurologic sequelae and consequences in wound healing [15], [16], [17]. Apart of these consequences, hypernatremia is associated with adverse outcomes in critically ill and severely burned patients [15], [18].
We conclude that serum sodium concentration can be used to control fluid removal strategy after burn shock. There is a systemic relevant coherence of amount and velocity of fluid removal and elevated serum sodium levels. There is a need of a well established fluid removal strategy in severely burned patient to avoid water and electrolyte imbalances.
Limitations
Because of the small population and sometimes different diuresis protocols used further investigation is recommended to figure out a safe method of fluid removal after burn injury. Choice and amount of administered diuretic agents to enforce diuresis, as well as a definition of daily IDR to minimize dehydration risk are not described in the literature.
Notes
Competing interests
The authors declare that they have no competing interests.
References
[1] Herndon T. Total burn care. 3. ed. Philladelphia: Saunders; 2007.[2] Gamelli RL, Paxton TP, O'Reilly M. Bone marrow toxicity by silver sulfadiazine. Surg Gynecol Obstet. 1993;177(2):115-20.
[3] Jarrett F, Ellerbe S, Demling R. Acute leukopenia during topical burn therapy with silver sulfadiazine. Am J Surg. 1978;135(6):818-9. DOI: 10.1016/0002-9610(78)90173-3
[4] Pham TN, Cancio LC, Gibran NS. American Burn Association practice guidelines burn shock resuscitation. J Burn Care Res. 2008;29(1):257-66.
[5] Baxter CR. Fluid volume and electrolyte changes of the early postburn period. Clin Plast Surg. 1974;1(4):693-703.
[6] Zawacki BE. Reversal of capillary stasis and prevention of necrosis in burns. Ann Surg. 1974;180(1):98-102. DOI: 10.1097/00000658-197407000-00015
[7] Namdar T, Stollwerck PL, Stang FH, Siemers F, Mailänder P, Lange T. Transdermal fluid loss in severely burned patients. Ger Med Sci. 2010;8:Doc28. DOI: 10.3205/000117
[8] Baxter CR, Shires T. Physiological response to crystalloid resuscitation of severe burns. Ann N Y Acad Sci. 1968;150(3):874-94. DOI: 10.1111/j.1749-6632.1968.tb14738.x
[9] Warden GD, Wilmore DW, Rogers PW, Mason AD, Pruitt BA Jr. Hypernatremic state in hypermetabolic burn patients. Arch Surg. 1973;106(4):420-7.
[10] Janz T. Sodium. Emerg Med Clin North Am. 1986;4(1):115-30.
[11] Lin M, Liu SJ, Lim IT. Disorders of water imbalance. Emerg Med Clin North Am. 2005;23(3):749-70. DOI: 10.1016/j.emc.2005.03.001
[12] Snyder NA, Feigal DW, Arieff AI. Hypernatremia in elderly patients. A heterogeneous, morbid, and iatrogenic entity. Ann Intern Med. 1987;107(3):309-19.
[13] Heimbach D, Engrav L, Grube B, Marvin J. Burn depth: a review. World J Surg. 1992;16(1):10-5. DOI: 10.1007/BF02067108
[14] Zellweger G, ed. Die Behandlung der Verbrennungen. Köln: Deutscher Ärzte Verlag; 1985.
[15] Fisher LA, Ko N, Miss J, Tung PP, Kopelnik A, Banki NM, Gardner D, Smith WS, Lawton MT, Zaroff JG. Hypernatremia predicts adverse cardiovascular and neurological outcomes after SAH. Neurocrit Care. 2006;5(3):180-5. DOI: 10.1385/NCC:5:3:180
[16] Hoorn EJ, Betjes MG, Weigel J, Zietse R. Hypernatraemia in critically ill patients: too little water and too much salt. Nephrol Dial Transplant. 2008;23(5):1562-8. DOI: 10.1093/ndt/gfm831
[17] Kuroda T, Harada T, Tsutsumi H, Kobayashi M. Hypernatremia deepens the demarcating borderline of leukocytic infiltration in the burn wound. Burns. 1997;23(5):432-7. DOI: 10.1016/S0305-4179(97)00016-8
[18] Polderman KH, Schreuder WO, Strack van Schijndel RJ, Thijs LG. Hypernatremia in the intensive care unit: an indicator of quality of care? Crit Care Med. 1999;27(6):1105-8. DOI: 10.1097/00003246-199906000-00029




