A COVID-19 outbreak with a high attack rate among inpatients in a psychiatric hospital in Wenzhou, China
Yiwei Zhou 1,2,3Xingbao Lin 4
Yu Huang 4
Chunhua Wu 4
Jun Li 5
Jieru Huang 5
Zumu Zhou 4
1 Business School, University of Shanghai for Science and Technology, Shanghai, China
2 School of Intelligent Emergency Management, University of Shanghai for Science and Technology, Shanghai, China
3 Smart Urban Mobility Institute, University of Shanghai for Science and Technology, Shanghai, China
4 The Affiliated Kangning Hospital of Wenzhou Medical University, Zhejiang Provincial Clinical Research Center for Mental Disorders, Wenzhou, China
5 Wenzhou Center for Disease Control and Prevention, Wenzhou, China
Abstract
Background: Since the emergence of COVID-19, China has taken strict prevention and control measures against the disease. At the end of 2022, when the government optimized and relaxed the COVID-19 prevention and control policy, a new wave of the epidemic appeared. This paper reports an outbreak of COVID-19 among inpatients in a psychiatric hospital in Wenzhou, China.
Methods: The case definition of COVID-19 was established. Throat swab specimens were collected and examined by RT-PCT. Questionnaires were distributed to hospitalized patients. Survey data were collected and analyzed.
Results: Of 902 inpatients in our hospital, 762 became infected with COVID-19, an attack rate of 84.5%. The outbreak occurred from 10 December, 2022 to January 18, 2023. Twenty patients died, yielding a case fatality rate of 2.6%. Most of the dead were among elderly people with underlying diseases, and 19 of the deceased were over 65 years old.
Conclusion: Our investigation showed that the outbreak of COVID-19 among hospitalized patients had the characteristics of high incidence, strong infectivity, and rapid transmission. Infectious sources were introduced into the hospital from the community and spread within the hospital, resulting in an outbreak. In addition, special attention should be paid to elderly people with underlying diseases when treating patients with COVID-19 in the future.
Keywords
COVID-19, outbreak, cluster, psychiatric hospital
Introduction
Since the emergence of COVID-19, outbreaks and epidemics of varying severity have occurred in various countries [1], [2]. The COVID-19 outbreaks have sometimes been reported in nursing homes, medical institutions, schools, shopping malls, families, fitness centers, and public venues [2], [3], [4], [5], [6], [7], [8]. Since the outbreak of COVID-19 in Wuhan, China has taken strict prevention and control measures, and the epidemic has been effectively controlled in scale and intensity. However, due to the close relations between China and other countries, the SARS-COV-2 mutant strains have been continuously imported, and sporadic cases or clusters of COVID-19 have often occurred throughout the country; for instance, Wenzhou has also experienced outbreaks of COVID-19 in family clusters and shopping malls [2], [5], as well as in many other regions and other medical institutions. Recently, a COVID-19 outbreak occurred in a psychiatric hospital in Wenzhou, China, at a time when the national measures for COVID-19 prevention and control were being adjusted, optimized, and relaxed. Immediately after the outbreak, we investigated the clinical and epidemiological characteristics of this COVID-19 outbreak to provide a basis for future responses to COVID-19 and similar outbreaks.
Methods
Case definition
COVID-19 cases hospitalized between December 8, 2022 and January 18, 2023 with a history of exposure to COVID-19 patients and with acute onset of fever and cough (ILI) or acute onset of three or more of the following symptoms: fever, cough, malaise, muscle aches, nasal congestion, runny nose, sore throat, decreased sense of smell and taste, diarrhea, and conjunctivitis [9]; or pulmonary imaging exhibited signs of pneumonia; or positive PCR test.
Questionnaire
Using a uniformly designed questionnaire, a nurse manager on each ward was responsible for the survey on their respective ward, asking questions, and recording the incidence and associated conditions of each inpatient between December 1, 2022, and January 30, 2023, including age, sex, time of onset, clinical symptoms, vaccination status, laboratory tests, chest CT and/or radiographic findings. Questionnaires were completed and returned. The collected data were analyzed using Excel software. All case investigations were performed by epidemiologists.
Laboratory tests: Throat swabs were collected from cases early in the outbreak and SARS-CoV-2 nucleic acid was detected by RT-PCR. Some outbreak cases were also selected for detection of SARS-CoV-2 antigen.
Statistical method
Statistical analysis was performed using Excel software. The Chi-square test was used for categorical variables. Statistical significance was set at P<0.05.
Ethical approval
The present survey was approved by the Medical Ethics Committee of The Affiliated Kangning Hospital of Wenzhou Medical University, Wenzhou, China (No 2023017). This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice. All participants gave informed consent. Before the survey was conducted, each patient was informed that the information collected in this survey would be kept confidential and would not be disclosed; the data were kept by a specifially designated person. The purpose and scope of the study were explained in the questionnaire at the beginning of the survey. A few sentences about voluntary informed consent were added at the beginning of the questionnaire. The patient was aware of the use of this information; if the patient was not willing to comply with the survey, they could not complete the questionnaire.
Results
Overview
The psychiatric hospital is a tertiary class-A hospital with 1,200 beds and more than 1,100 employees,integrating medical treatment, teaching and rehabilitation. It has an inpatient and an outpatient department. The inpatient department has 19 wards, including comprehensive ward, child and adolescent psychology ward, sleep medicine ward, clinical psychology ward, early mental intervention ward, psychosomatic disorders ward, emotional disorders ward, behavioral medicine ward, memory disorders ward, geriatric psychiatry ward, women’s psychiatry ward, general psychiatry ward, and special care ward. Patients in the special care ward are usually widowed elderly people with long hospital stays and financial difficulties, who have received little care from their families and belong to vulnerable groups.
Distribution over time
During the COVID-19 outbreak, 902 patients were hospitalized between December 10, 2022, and January 18, 2023, of whom 762 became ill (attack rate 84.48%). The first case occurred on December 10, 2022, followed by a succession of sporadic cases until December 16, with a gradual increase after December 17 and more than 100 cases per day from December 19 to 22, reaching peak incidence. This was followed by a gradual decrease until January 18, 2023, when the outbreak was terminated. The number of cases from December 19 to 22 accounts for 63.25% of the total number of cases in this hospital. For temporal distribution of COVID-19 cases in the psychiatric hospital, see Figure 1 [Fig. 1].
Figure 1: Temporal distribution of 762 COVID-19 cases in the psychiatric hospital from December 2022 to January 2023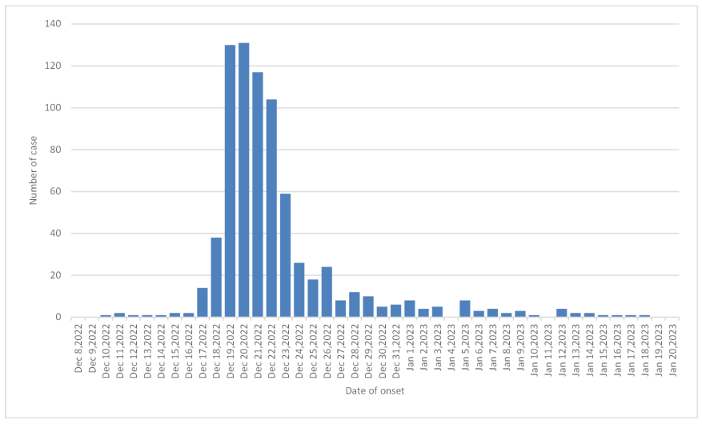
Distribution of cases by ward
The infection rate of COVID-19 was 100% in the comprehensive ward, child and adolescent psychiatry ward, clinical psychology ward, memory disorders ward I, and memory disorders ward III, while the lowest incidence rate was 58.90% in the women’s psychiatry ward. The difference in COVID-19 attack rates between wards was significant (χ2=115.02, P<0.01; Table 1 [Tab. 1]).
Table 1: COVID-19 attack rate among inpatients by ward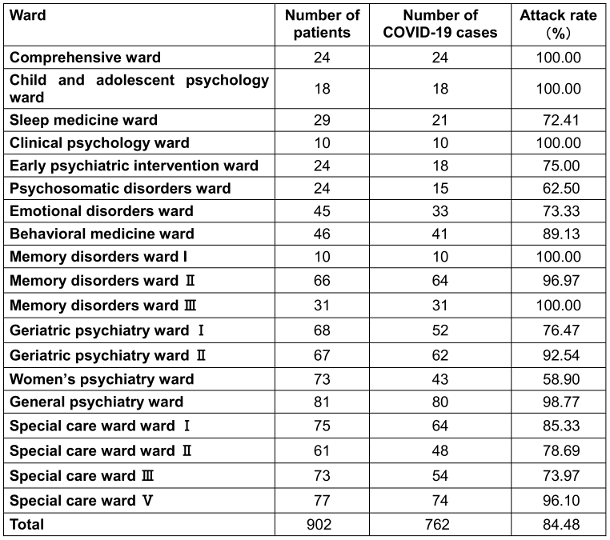
Attack rate by population
Among 902 subjects, 762 cases were affected. The overall attack rate of COVID-19 was 84.5% with males making up 88.39% of these, and females 78.1%, a highly stastistically significant difference (χ2=17.25, P<0.01). In terms of age, the highest attack rate was 96.3% in the group aged 75–79 years and the lowest was 76.5% in the group aged 30–39 years. When these cases were divided into groups ≤59 years of age and ≥60 years of age, the attack rates were 80.3% and 88.2% respectively. (χ2=4.18, P<0.05, Table 2 [Tab. 2]).
Table 2: Attack rate of COVID-19 by gender and age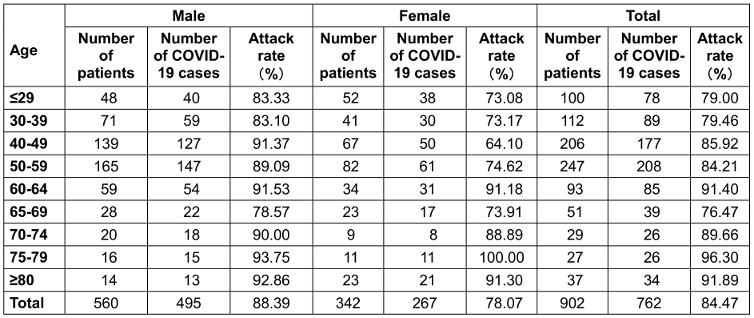
Clinical manifestations
Fever was proportionally higher than other symptoms, accounting for 96.1%; the other symptoms in decreasing order were dry cough, malaise, nasal congestion, sore throat and runny nose, accounting for 75.6%, 62.1%, 50.1%, 38.6% and 38.3%, respectively, while the proportion of loss of taste or smell, myalgia, diarrhea and conjunctivitis was lower (Table 3 [Tab. 3]).
Table 3: Proportion of various clinical manifestations of 762 COVID-19 cases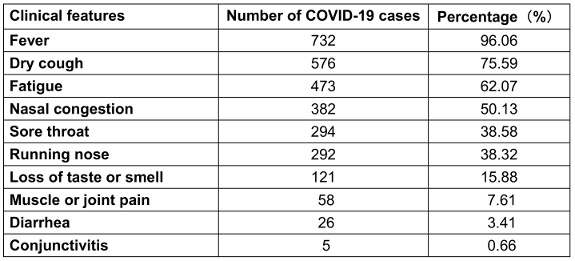
Cases of death
Between December 21, 2022 and January 20, 2023 out of the 762 COVID-19 cases, there were 20 deaths, 13 male and 7 female (a case fatality rate of 2.6%). With the exception of one 55-year-old patient, the remaining 19 deaths were over 65 years of age (of which three were 65–69, seven were 70–79, six were 80–89 and three were ≥90 years of age). Seventeen (17) deaths were due to pulmonary infection, one to myocarditis, one to uremia, and one to gastrointestinal bleeding. All three patients with myocarditis, uremia, or gastrointestinal bleeding were nucleic-acid positive by RT-PCR. Complications and/or comorbidities of these deaths included mental disorders (e.g, Alzheimer’s disease, schizophrenia, epileptic psychosis, epilepsy, delirium, vascular dementia, psychotic disorder, etc.) and chronic obstructive pulmonary disease (COPD), hypertension, type 2 diabetes mellitus, anemia, renal insufficiency, sequelae of cerebral infarction, osteoporosis, lacunar cerebral infarction, chronic hepatitis B, cholecystitis, chronic bronchitis, and other diseases.
Vaccination status of inpatients
After the COVID-19 outbreak, the COVID-19 vaccination status of hospitalized inpatients was investigated. Among the 902 cases investigated, 141 cases (15.6%) had been vaccinated with COVID-19 vaccine, including 11 cases (1.2%) with 1 dose of vaccine, 48 cases (5.3%) with 2 doses, 82 cases (9.1%) with 3 doses or more, 752 cases (83.4%) without vaccination, and 9 cases (1%) with unknown vaccination status. Among the 286 patients in the special care ward, only 1 case was fully vaccinated, i.e., the full vaccination rate was 0.4%; among the 616 cases in the non-special care ward, 139 cases were fully vaccinated, i.e., the full vaccination rate was 22.6%. The difference in the full vaccination rate between the special care wards and non-special care wards was highly significant (χ2=67.14, P<0.01). There were 130 cases with full vaccination (2 or more doses), of which 85 cases were morbid, an attack rate of 65.4%; 752 cases were not vaccinated, of which 662 cases were confirmed with COVID-19, i.e., an attack rate of 88%. The difference in attack rate between the full vaccination group and the non-vaccination group was highly significant (χ2=43.85, P<0.01, Table 4 [Tab. 4]).
Table 4: Vaccination rate of COVID-19 patients by ward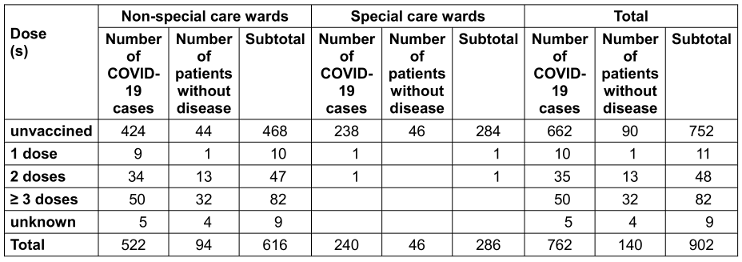
Prevention and control measures
After the outbreak, the hospital reacted quickly and took various prevention and control measures: doctors and nurses were instructed to closely monitor the change of the patient's condition and make all preparations for treatment; at the same time, personal protection to prevent and control the infection of medical personnel was comprehensively implemented; the hospital's emergency plan was activated. The laboratory and radiology departments worked overtime to produce test results as quickly as possible to provide physicians with timely diagnosis and treatment advice; patients were isolated; infected areas were disinfected; windows were opened for ventilation; and hand hygiene was reinforced. Staff access management was optimized and internal zoning management was implemented based on facility conditions.
Discussion
Over the past three years, governments at all levels have attached great importance to strict prevention and control measures against the COVID-19 pandemic and have expended a great deal of human and material resources to prevent and control the occurrence and spread of COVID-19, which has affected social development and economic operation as well as people’s daily lives, while effectively controlling the pandemic. It would be impractical and difficult to maintain these stringent prevention and control measures in the long term. In addition, in view of the mass vaccination with COVID-19 vaccine, the mutation of the SARS-COV-2 strain, the results of monitoring the predominant strain of SARS-COV-2, the existing experience in the prevention and control of COVID-19 at home and abroad, and the available medical and health resources, China has recently adjusted and optimized the prevention and control measures for COVID-19.
While the COVID-19 prevention and control measures were being adjusted and optimized, COVID-19 outbreaks occurred in most areas of China, and COVID-19 outbreaks also occurred in many local medical institutions. As a specialized hospital for the treatment of psychiatric and elderly patients, despite having taken many measures to prevent and control COVID-19, it was not spared from a COVID-19 outbreak. This survey confirmed the outbreak of COVID-19 among hospitalized patients in a psychiatric hospital based on epidemiology, clinical characteristics, and laboratory tests. The investigation showed that the source of infection of the outbreak was from the community. There were a large number of infectious sources in the community, enabling the virus to spread to the hospital. In this period of policy adjustment, the number of COVID-19 cases occurring in the community has increased rapidly, and it was difficult to control them effectively in a short period of time. As some outpatients carring SARS-CoV2 from the community came to our hospital for consultation and treatment, the virus was brought into the hospital and spread widely there, forming an outbreak. The present investigation showed that the first COVID-19 case in the COVID-19 outbreak in the psychiatric hospital occurred on December 10, 2022. According to a follow-up investigation, RT-PCR-positive nucleic-acid cases were identified in the outpatient laboratory of the hospital on December 8 and 9. In fact, before the outbreak, there were also some sporadic cases of COVID-19 in the local community where some outbreak-associated patients lived. Our survey showed that COVID-9 cases in the hospital were prevalent in the latter phase of the spread of the disease in the community, which was consistent with the results reported by Imamura et al [10]. However, the underlying mechanisms for the trend might differ between different medical institutions and countries.
In addition, the cause of outbreaks among psychiatric hospital inpatients may be related to the following factors. Psychiatric and elderly patients are highly susceptible to COVID-19 [11], [12], [13], and this high susceptibility is closely related to high infectivity and severe consequences. In addition, the patients admitted to this hospital are often older. The proportion of elderly and mentally ill patients in the hospital is high, and there are many patients with underlying diseases. Their immunity is weaker than that of younger, healthier individuals. In addition, the rate of COVID-19 vaccination among the elderly patients is very low; all of these factors contributed to the outbreak.
Ng et al. [14] reported that the attack rate of patients in six COVID-19 outbreaks in hospitals was 21.4±16.3%. In the United Kingdom, 5%–7% of COVID-19 cases have been reported to be associated with nosocomial infections [12]. A prospective study in a teaching hospital in London showed that 15% of COVID-19 cases were definitely or probably associated with nosocomial infections [15]. The present investigation showed an attack rate of 84.47% among hospitalized patients, which is higher than that reported by other investigators [12], [14], [15]. Ng et al. [14] reported 28 COVID-19 outbreaks at various hospitals, with a case fatality rate of 15.0±20.7%. Abbas et al. [15] reported that a case fatality rate of 36% for COVID-19 patients at the teaching hospital in London. In another study of COVID-19 outbreak, the COVID-19 case fatality rate was as high as 50.0% in patients with underlying blood disorders [14]. The present study showed that the COVID-19 case fatality rate among psychiatric hospital inpatients was 2.6%, which was lower than that reported in other studies [14], [15]. Additionally, The current investigation of the COVID-19 outbreak showed that most of these deaths were of patients with underlying medical conditions, including mental disorders (e.g., Alzheimer’s disease, schizophrenia, epileptic psychosis, epilepsy, delirium, vascular dementia, psychotic disorders, etc.), chronic obstructive pulmonary disease (COPD), hypertension, type 2 diabetes mellitus, anemia, renal insufficiency, cerebral infarction sequelae, osteoporosis, lacunar cerebral infarction, chronic hepatitis B, cholecystitis, chronic bronchitis and other diseases, thus increasing the susceptibility of patients and the severity of the disease, so patients with these underlying diseases should be very closely monitored.
Some studies have shown that SARS-COV-2 is mainly transmitted by respiratory droplets and close contact [16], [17]. The epidemiological investigation of this outbreak showed that many individuals with COVID-19 were present in the community prior to this COVID-19 outbreak at our hospital, and several RT-PCR nucleic acid-positive specimens were detected among outpatients from the community. These RT-PCR-positive outpatients moved between the outpatient and inpatient units, and person-to-person transmission by respiratory droplets was ongoing. Consequently, infected patients on the ward could also transmit COVID-19 to the other inpatients through close contact. In addition, the Omicron variant has become the predominant strain in China and elsewhere. Information obtained from the Wenzhou Center for Disease Control and Prevention shows that the locally prevalent SARS-COV-2 strain is the omicron strain, which is highly transmissible [18], [19]. This strain caused an 84.5% attack rate among hospitalized patients in the present COVID-19 outbreak. After the first few cases occurred in some wards, COVID-19 quickly spread to other patients in the same wards, resulting in cross-contamination. All wards were eventually affected, and in some, all became ill. In addition, the Omicron strain spreads rapidly [20]; the number of cases in the UK increased exponentially every 2–3 days [18]. At the peak of the current outbreak, 482 people became ill in just 4 days, representing 63.3% of the total number of cases. Thus, this outbreak caused by the Omicron strain is not only highly transmissible but also rapidly spreading. The causative agent of this outbreak was identified as Omicron strain BF.5 by the Wenzhou Center for Disease Control and Prevention.
In this COVID-19 outbreak, 20 patients died, i.e., a case fatality rate of 2.62%, because they had not been previously vaccinated. The vast majority of infected patients were unvaccinated and some had multiple comorbidities. As a result, these patients were highly susceptible due to their lack of immunity or decreased resistance to viral infection; once infected, they were often prone to severe illness and death [21]. Studies have shown that the fatal cases were mainly elderly, high-risk individuals with underlying diseases [22]. Our survey showed that the deceased in this COVID-19 outbreak were older people. Of these deaths, 80% were over 70 years, and 45% were over 80 years of age. Most of these nucleic acid-positive deaths confirmed by RT-PCR were due to pulmonary infections, while a few patients died of sudden death, uremia, and gastrointestinal bleeding. Therefore, priority should be given to improving the protection of the elderly during COVID-19 outbreaks, especially the lonely elderly and vulnerable elderly with comorbidities. Therefore, adequate medical resources should be provided for these high-risk groups, and hospitals should be well prepared for the comorbidity and mortality of these elderly people as a result of COVID-19 infection.
Most of the patients in the special care ward are elderly widows who have been hospitalized for a long time. Since their families rarely take care of them for various reasons, these patients mainly live on financial support from the government. The current survey showed that they did not receive COVID-19 vaccinations in the local community in the time before hospitalization, and thus their vaccination rate was low. Among the 284 cases hospitalized for special care, most were unvaccinated; only 2 cases were vaccinated against COVID-19, with a vaccination rate of 0.70%. These vulnerable populations should be vaccinated with a safe and effective COVID-19 vaccine in the future to improve their immunity.
Limitations
Since this survey was an observational survey of a public health emergency, there will be some limitations. During this investigation, RT-PCR nucleic-acid testing or SARS-CoV-2 antigen examination was not performed on individuals without clinical symptoms. Some of these cases without clinical symptoms may actually be infected, which may also play an important role in the transmission process. In addition, the local vaccinations against COVID-19 prior to the outbreak were Sinovac-CoronaVac vaccine and SinoPharm-Beijing BBIBP-CorV vaccine. When the COVID-19 vaccination of patients was surveyed, it was difficult to distinguish which COVID-19 vaccine was administered to the recipients.
Conclusion
Our investigation showed that the outbreak of COVID-19 among hospitalized patients in a psychiatric hospital had the characteristics of high incidence, strong infectivity, and rapid transmission at the end of 2022, when the government of China adjusted and optimized the COVID-19 prevention and control policy. Infectious sources were introduced into the hospital from the community and spread within the hospital, resulting in an outbreak. In the future, special attention should be paid to the elderly with underlying diseases when treating patients with COVID-19.
Notes
Competing Interests
The authors declare that they have no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to express out heartfelt gratitude to all staff at The Affiliated Kangning Hospital of Wenzhou Medical University who were involved in the investigation.
Funding
This work was supported by 2022 Ministry of Education of China Humanities and Social Science Youth Foundation Project (22YJC790189); Shanghai Key Laboratory of Urban Design and Urban Science, NYU Shanghai Open Topic Grants (Grant No.2023YWZHOU_LOUD).
Availability of data and materials
The datasets used and analyzed in this study are available from the corresponding author on reasonable request.
Authors’ ORCID-ID
- Yiwei Zhou: 0000-0002-4625-6875
- Zumu Zhou: 0000-0002-5526-7808
References
[1] Kim SW. COVID-19 Outbreak in Daegu City, Korea and Response to COVID-19: How Have We Dealt and What Are the Lessons? J Korean Med Sci. 2022 Dec 26;37(50):e356. DOI: 10.3346/jkms.2022.37.e356[2] Zhou Y, Xiang F, Ni C, Zhang X, Xie H, Zhu H, Zhou Z. Travel-associated outbreak of COVID-19 in a departmental store, Wenzhou, China. J Infect Dev Ctries. 2022 May 30;16(5):752-58. DOI: 10.3855/jidc.15670
[3] Suhs T, Gerlach D, Garfin J, Lorentz A, Firestone M, Sherden M, Hackman K, Gray T, Siebman S, Wienkes H, Vilen K, Wang X, Como-Sabetti K, Danila R, Smith K, Medus C. COVID-19 Outbreak Associated With a Fitness Center-Minnesota, September-November 2020. Clin Infect Dis. 2022 Apr 9;74(7):1265-7. DOI: 10.1093/cid/ciab653
[4] Zoghbi M, Haddad C, Khansa W, Karam E, Chamoun A, Hachem D. COVID-19 outbreak in a psychiatric hospital: what makes it worse? Ann Gen Psychiatry. 2022 Jul 11;21(1):26. DOI: 10.1186/s12991-022-00403-4
[5] Zhou ZM, Zhou HZ, Lin XD, Su ZC, Zhao LS, Chen X. Outbreak of COVID-19 in a family, Wenzhou, China. Epidemiol Infect. 2020 May 20;148:e103. DOI: 10.1017/S0950268820001089
[6] Taylor J, Carter RJ, Lehnertz N, Kazazian L, Sullivan M, Wang X, Garfin J, Diekman S, Plumb M, Bennet ME, Hale T, Vallabhaneni S, Namugenyi S, Carpenter D, Turner-Harper D, Booth M, Coursey EJ, Martin K, McMahon M, Beaudoin A, Lifson A, Holzbauer S, Reddy SC, Jernigan JA, Lynfield R; Minnesota Long-Term Care COVID-19 Response Group. Serial Testing for SARS-CoV-2 and Virus Whole Genome Sequencing Inform Infection Risk at Two Skilled Nursing Facilities with COVID-19 Outbreaks - Minnesota, April-June 2020. MMWR Morb Mortal Wkly Rep. 2020 Sep 18;69(37):1288-95. DOI: 10.15585/mmwr.mm6937a3
[7] Boudhabhay I, Serris A, Servais A, Planas D, Hummel A, Guery B, Parize P, Aguilar C, Dao M, Rouzaud C, Ferriere E, Knebelmann B, Sakhi H, Leruez M, Joly D, Schwartz O, Lanternier F, Bruel T. COVID-19 outbreak in vaccinated patients from a haemodialysis unit: antibody titres as a marker of protection from infection. Nephrol Dial Transplant. 2022 Jun 23;37(7):1357-65. DOI: 10.1093/ndt/gfac016
[8] van Ewijk CE, Hazelhorst EI, Hahné SJM, Knol MJ. COVID-19 outbreak in an elderly care home: Very low vaccine effectiveness and late impact of booster vaccination campaign. Vaccine. 2022 Nov 2;40(46):6664-9. DOI: 10.1016/j.vaccine.2022.09.080
[9] World Health Organization. WHO COVID-19 Case definition: Updated in Public health surveillance for COVID-19. 2022 Jul 22 [accessed 2023 Feb 25]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2022-1
[10] Imamura T, Ko YK, Furuse Y, Imamura T, Jindai K, Miyahara R, Sando E, Yasuda I, Tsuchiya N; Field Epidemiology Training Program, Japan (FETP-J), The National COVID-19 Cluster Response Taskforce; Saito M, Suzuki M, Oshitani H. Epidemiological Factors Associated with COVID-19 Clusters in Medical and Social Welfare Facilities. Jpn J Infect Dis. 2022 May 24;75(3):281-7. DOI: 10.7883/yoken.JJID.2021.288
[11] Druss BG. Addressing the COVID-19 Pandemic in Populations With Serious Mental Illness. JAMA Psychiatry. 2020 Sep 1;77(9):891-2. DOI: 10.1001/jamapsychiatry.2020.0894
[12] Shinn AK, Viron M. Perspectives on the COVID-19 Pandemic and Individuals With Serious Mental Illness. J Clin Psychiatry. 2020 Apr 28;81(3):20com13412. DOI: 10.4088/JCP.20com13412
[13] Paruk S, Ngcobo NN, Karim E, Tomita A, Ramlall S. COVID-19 infection at a psychiatric hospital in KwaZulu-Natal, South Africa: Clinical service planning and challenges. S Afr J Psychiatr. 2022 Dec 7;28:1933. DOI: 10.4102/sajpsychiatry.v28i0.1933
[14] Ng CYH, Lim NA, Bao LXY, Quek AML, Seet RCS. Mitigating SARS-CoV-2 Transmission in Hospitals: A Systematic Literature Review. Public Health Rev. 2022 Feb 23;43:1604572. DOI: 10.3389/phrs.2022.1604572
[15] Abbas M, Robalo Nunes T, Martischang R, Zingg W, Iten A, Pittet D, Harbarth S. Nosocomial transmission and outbreaks of coronavirus disease 2019: the need to protect both patients and healthcare workers. Antimicrob Resist Infect Control. 2021 Jan 6;10(1):7. DOI: 10.1186/s13756-020-00875-7
[16] Ghinai I, McPherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K, Rubin R, Morales-Estrada S, Black SR, Pacilli M, Fricchione MJ, Chugh RK, Walblay KA, Ahmed NS, Stoecker WC, Hasan NF, Burdsall DP, Reese HE, Wallace M, Wang C, Moeller D, Korpics J, Novosad SA, Benowitz I, Jacobs MW, Dasari VS, Patel MT, Kauerauf J, Charles EM, Ezike NO, Chu V, Midgley CM, Rolfes MA, Gerber SI, Lu X, Lindstrom S, Verani JR, Layden JE; Illinois COVID-19 Investigation Team. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. 2020 Apr 4;395(10230):1137-44. DOI: 10.1016/S0140-6736(20)30607-3
[17] Hamner L, Dubbel P, Capron I, Ross A, Jordan A, Lee J, Lynn J, Ball A, Narwal S, Russell S, Patrick D, Leibrand H. High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice - Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020 May 15;69(19):606-10. DOI: 10.15585/mmwr.mm6919e6
[18] Araf Y, Akter F, Tang YD, Fatemi R, Parvez MSA, Zheng C, Hossain MG. Omicron variant of SARS-CoV-2: Genomics, transmissibility, and responses to current COVID-19 vaccines. J Med Virol. 2022 May;94(5):1825-32. DOI: 10.1002/jmv.27588
[19] Fan Y, Li X, Zhang L, Wan S, Zhang L, Zhou F. SARS-CoV-2 Omicron variant: recent progress and future perspectives. Signal Transduct Target Ther. 2022 Apr 28;7(1):141. DOI: 10.1038/s41392-022-00997-x
[20] Mohsin M, Mahmud S. Omicron SARS-CoV-2 variant of concern: A review on its transmissibility, immune evasion, reinfection, and severity. Medicine (Baltimore). 2022 May 13;101(19):e29165. DOI: 10.1097/MD.0000000000029165
[21] Müller-Wieland D, Marx N, Dreher M, Fritzen K, Schnell O. COVID-19 and Cardiovascular Comorbidities. Exp Clin Endocrinol Diabetes. 2022 Mar;130(3):178-89. DOI: 10.1055/a-1269-1405
[22] Shakor JK, Isa RA, Babakir-Mina M, Ali SI, Hama-Soor TA, Abdulla JE. Health related factors contributing to COVID-19 fatality rates in various communities across the world. J Infect Dev Ctries. 2021 Sep 30;15(9):1263-72. DOI: 10.3855/jidc.13876




