[Calculated parenteral initial therapy of bacterial infections: Antibiotic treatment in the elderly]
Peter Walger 1,2,3Hans Jürgen Heppner 4
1 Hygiene, Infektionsmanagement und ABS, Bonn, Germany
2 Johanniter GmbH Berlin, Germany
3 Verbund Katholischer Kliniken Düsseldorf, Germany
4 Geriatrische Klinik und Tagesklinik, Helios Klinikum Schwelm, Germany
Abstract
This is the fifteenth chapter of the guideline “Calculated initial parenteral treatment of bacterial infections in adults – update 2018” in the 2nd updated version. The German guideline by the Paul-Ehrlich-Gesellschaft für Chemotherapie e.V. (PEG) has been translated to address an international audience.
Multimorbidity, an atypical symptomatology of infections in combination with multimedication, the associated interaction risks and serious consequences of synergistic side effects characterize the conditions when deciding on the use of antibiotics in old age. Strict decision regarding the indication itself, choice of the best antibiotic even considering rare side effects which may be dangerous in the elderly, determining the correct dose, dosing interval and the shortest possible duration according to the physiological status of the patient as well as monitoring effectiveness and toxicity detect expected and unexpected side effects early. Recommendations must reflect the peculiarities of antibiotic treatment in elderly patients.
Introduction
The aging population means that the composition is shifting more and more towards older people. By 2050, it is estimated the proportion of over-65s will be at 30–40%, while at the same time the share of very elderly people (80 years and older) will rise to 15%, almost trebling [1]. This demographic change is leading to an increase in geriatric patients in all areas of medical care. So it is very important to know the basic definition of what constitutes a geriatric patient (see Table 1 [Tab. 1]).
Table 1: Definition of the geriatric patient [46]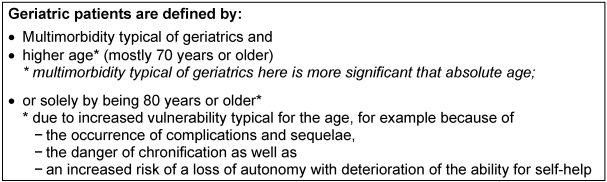
The proportion of 90-year-old patients requiring acute care is also increasing, for example in cardiac surgery [2] or geriatric trauma [3]. This requires a high level of geriatric expertise in care if it is necessary to treat concomitant or complicating infections in this vulnerable patient group [4]. Under adequate treatment the outcome is good while maintaining the patient’s functional level [5]. It is therefore important to have a basic understanding of the peculiarities of anti-infective treatment in the elderly.
Multimorbidity, i.e. the simultaneous presence of several chronic diseases in need of treatment, consequently leads to multimedication and thus to the risk of synergistic side effects and undesirable interactions in antibiotic treatment.
In addition to the physiological changes in the aging human body, immune senescence also leads to a greater susceptibility to infection in this patient group. Morbidity and mortality of many infectious diseases increase with age. Infections are a major cause of death in older patients [6].
The most common cause of infection-related death in patients >65 years of age is community-acquired pneumonia (CAP), with long-term care and in particular being bed-ridden significantly increasing the risk of death [7]. Numerous other infections such as urinary tract infections, sepsis, skin and soft tissue infections, bacterial endocarditis, cholecystitis and diverticulitis show increasing incidences. Atypical clinical manifestations, for example by weakening of the fever reaction, nonspecific general symptoms or early impairments of brain function make the diagnosis more difficult and delay timely and adequate treatment [8], [9], [10].
Older patients with bacterial infections have different clinical characteristics compared to younger patients due to their limited local and systemic responses to an infection. Symptoms of acute infection in elderly patients are usually “nonspecific” and “atypical”. Fever, the cardinal symptom of a bacterial infection, is absent in over 30% of cases [11]. The usual lab markers for the detection of an infection, such as leukocyte count or C-reactive protein (CRP), may initially also be normal or only minimally altered [12]. CRP and white blood cell counts are therefore unreliable parameters in geriatric patients [13].
Key on antibiotic-associated side effects in old age
Physiological changes affect pharmacokinetics in old age. This concerns both the release and absorption of drugs as well as their distribution through the changes to fat and water mass in old age and the (mainly renal) drug elimination. A summary of the most important age-related changes affecting the pharmacokinetics of anti-infective agents is shown in Table 2 [Tab. 2].
Table 2: Pharmacokinetics and physiological aging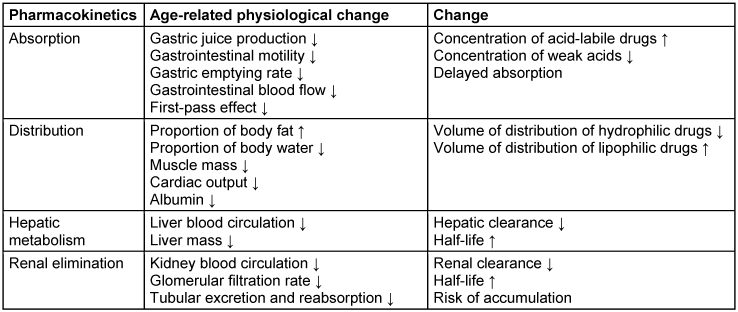
Over 30% of people >70 years old have at least five chronic diseases [10]. Extensive use of prescribed and over-the-counter (OTC) medication and herbal preparations is typical of the elderly. For example, 25% of women over the age of 65 (in the US) take five prescribed medications and 12% use ten or more medications. This inevitably increases the risk of complications [14].
The data for Germany are similar. People over the age of 70 take an average of three different medicines per day; those aged 80 to 85 receive the highest number per day [15], 35% of those >70-year-olds receive 5 to 8 and 15% more than 13 different drugs [16]. Of the elderly studied, 14% (in 1998) also took additional herbal or other dietary supplements [17]; in 2002 this figure was 26–27% [18], [19].
A fictitious 79-year-old patient with five of the most common comorbidities (COPD, type 2 diabetes mellitus, hypertension, osteoporosis, osteoarthritis) receives 12 drugs a day according to guidelines (USA 2005), following complicated rules for administration with unpredictable interactions between diseases and medications and with numerous adverse drug reactions [20].
Side effects of medications are generally up to 3 times more common in elderly patients compared to 30 year olds [21]. When taking up to 5 medications, there is a 4% risk of ADR (adverse drug effects), with 6–10 medications this risk is 10% and with 11–15 medications 28% [22].
Overall, ADRs are found in 14.6–35% of elderly patients. 20–25% of geriatric in-patient admissions are the result of ADRs. Anticoagulants, nonsteroidal anti-inflammatory drugs (NSAIDs), antidiabetics, diuretics and digitalis glycosides are most commonly associated with ADRs that lead to hospital admission [23]. Interactions play a role in around 40% of ADRs. Low body weight is associated with ADRs especially often. Over 80% of ADR-associated in-patient admissions are preventable [24], [25].
Prevalence of inadequate regulations
Data from the US, Canada and Europe show a high proportion of “potentially inadequate medications” (PIM) in elderly patients, for example in the USA 1994: 23.5% USA 1996 20% – of which 3% from the Beers list, historically the first published PIM list – of the 11 “always avoid” drugs with increased risk of hospitalization and death), USA 2002: 19% Europe 2005: ~20%. The typical polypharmacy patient with an increased incidence of inadequate medication is female, >85 years old, living alone and has low health and social status [26], [27].
The Beers Criteria [28] include a list of inadequate medications consisting of three groups: “always avoid” (11 drugs), “rarely appropriate” (8 drugs) and “some indication but often misused” (14 drugs). Based on these criteria, revised PIM lists have been published in the US, France, the Netherlands and Canada [29], [30], [31], [32]. The risk of ADR leading to in-patient admission of elderly patients is therefore particularly high if several medicines are taken at the same time (risk of interaction). Multimedication, prescription of neuroleptics or anti-dementia drugs are significant risk factors for ADRs in nursing home residents [33]. The PRISCUS list has been tailored to the conditions in Germany. It comprises 83 drugs from 18 different drug classes, hailing from a wide range of treatment areas, that are considered potentially unsuitable for senior citizens [34], [35]. However, there is no definite position on antibiotics with the exception of nitrofurantoin.
Polypharmacy generally increases the risk of adverse events and increases the risk of clinically relevant drug interactions. This is also described for some anti-infective drugs which are added to existing multi-medication. To minimize these potential risks, this issue should receive increased attention in making decisions about anti-infective drug treatment.
The treatment of elderly patients with a bacterial infectious disease therefore typically means adding a further substance, an antibiotic, to a long list of different medications with a partially unclear potential for interactions and various ADRs, which may themselves have their own side effects as well as their own potential for interactions.
This can then quickly lead to situations requiring treatment and that are sometimes life-threatening [36].
Antibiotic prescriptions for elderly patients
The assessment of the different classes of antibiotics (or individual substances thereof) is based on specific aspects and risks adapted to the age of the patient (see Table 3 [Tab. 3]).
Table 3: Evaluation of the individual antibiotic classes or individual substances according to side effects and risk of interactions in elderly patients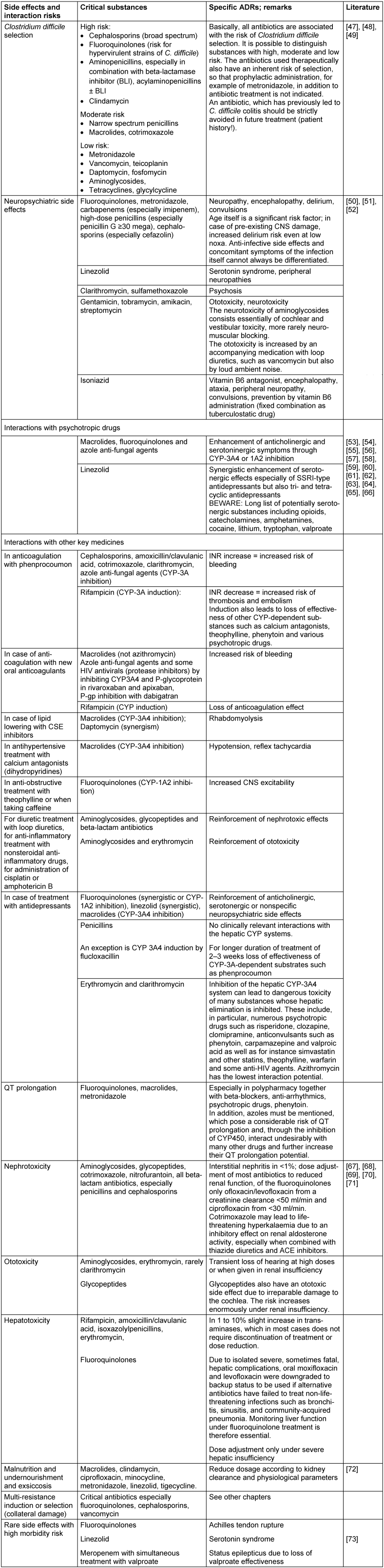
Assessment of renal function in old age
Changes to renal elimination represent the most clinically significant change in body function in terms of pharmacokinetic effects on drugs and is inevitably associated with increasing age [37]. The average renal blood flow decreases by about 10% per decade of age from 600 ml/min per 1.73 m2 in the 4th decade to about 300 ml/min per 1.73 m2 in the 9th decade. At the same time, the glomerular filtration rate decreases by about 10% per decade. At the same time, as creatinine production decreases with age as a result of the progressive loss of muscle mass, the serum creatinine level remains constant. Creatinine levels in the upper normal range therefore indicate an already existing restriction of kidney function. An increase in serum creatinine should be given special consideration when determining antibiotic dosages. Many labs report the Glomerular Filtration Rate (GFR) based on calculation using the MDRD (Modification of Diet in Renal Disease Study) formula. However, this formula was not validated in the MDRD study regarding people over the age of 70. The alternative formula according to Cockcroft-Gault shows significant limitations of the GFR calculation depending on the age and large variances of the body weight. In comparative studies, GFR estimates based on a 24-hour composite urine sample showed the best results, albeit with a tendency to overestimate. In practice, however, there are significant limitations of the method due to collection errors. Another alternative is the determination of cystatin C, which is characterized by independence from age and muscle mass [38], although discussion of this parameter is also controversial [39]. This method seems to be most reliable in cases of incipient kidney function restriction where there is still no increase in creatinine. Overall, all methods of determining renal function in the elderly have clear limitations. An overestimation of the glomerular filtration rate should therefore be compensated for by a cautious use of potentially nephrotoxic substances [40].
Antibiotic resistance in old age
All factors associated with the risk of colonization or infection by multidrug-resistant agents are becoming increasingly important in old age. Multimorbidity and specific comorbidities such as diabetes mellitus or COPD, previous antimicrobial treatment, prior hospital stays, being cared for in nursing homes, rehabilitation facilities and other tertiary care structures, carriers of invasive devices such as enteral feeding tubes, central venous indwelling catheters, tracheostomy and urinary catheters, other out-patient nosocomial risks such as dialysis, chronic ulcers or other long-term care and pre-existing colonization accumulate with increasing age. As expected, residents of nursing homes show an increased incidence of resistant pathogens, depending on their functional limitations [41], [42]. The risk of multidrug resistance in the case of an infection poses special requirements for the prescription of adequate antibiotic treatment, be it through the selection of a suitable broad-spectrum antibiotic or through a suitable combination strategy. With inadequate treatment, there is a risk of prolonged hospitalization, increased costs and, in the worst case, increased hospital mortality [43], [44]. The risk of multidrug resistance has to be assessed individually, a general assumption of an age-related increased risk of MRE without appreciation of the individual risk factors leads to inadequate over-treatment with broad-spectrum antibiotics.
Summary
In principle, the use of antibiotics in elderly patients can be based on the same principles as for younger people. There is no antibiotic which in principle must be regarded as inadequate for older people.
However, the choice and dosage of antibiotics must be adjusted to the general medical problems of old age in conjunction with the physiological changes. The increased risk of resistant and multi-drug resistant infectious pathogens as a result of multiple hospital stays and prior antibiotic treatment has become an increasingly prominent issue in recent years.
Due to the more frequent and potentially serious consequences of antibiotic side effects (adverse drug reactions, ADRs) in older compared to younger patients, the following steps for optimization are essential: Strict decision regarding the indication itself, choice of the best antibiotic even considering rare side effects which may be dangerous in the elderly, determining the correct dose, dosing interval and the shortest possible duration according to the physiological status of the patient as well as monitoring effectiveness and toxicity detect expected and unexpected side effects early. In geriatric patients their frailty carries a great risk of developing a complicated progression with more difficult convalescence and higher mortality [45]. Therefore, recommendations must reflect the peculiarities of antibiotic treatment in elderly patients.
Note
This is the fifteenth chapter of the guideline “Calculated initial parenteral treatment of bacterial infections in adults – update 2018” in the 2nd updated version. The German guideline by the Paul-Ehrlich-Gesellschaft für Chemotherapie e.V. (PEG) has been translated to address an international audience.
Competing interests
The authors declare that they have no competing interests.
References
[1] Tesch-Römer C, Engstler H, Wurm S. Altwerden in Deutschland. Wiesbaden: VS Verlag für Sozialwissenschaften; 2006. DOI: 10.1007/978-3-531-90138-1[2] Afilalo J, Steele R, Manning WJ, Khabbaz KR, Rudski LG, Langlois Y, Morin JF, Picard MH. Derivation and Validation of Prognosis-Based Age Cutoffs to Define Elderly in Cardiac Surgery. Circ Cardiovasc Qual Outcomes. 2016 Jul;9(4):424-31. DOI: 10.1161/CIRCOUTCOMES.115.002409
[3] Stenqvist C, Madsen CM, Riis T, Jørgensen HL, Duus BR, Lauritzen JB, van der Mark S. Orthogeriatric Service Reduces Mortality in Patients With Hip Fracture. Geriatr Orthop Surg Rehabil. 2016 Jun;7(2):67-73. DOI: 10.1177/2151458515625296
[4] Beckett CL, Harbarth S, Huttner B. Special considerations of antibiotic prescription in the geriatric population. Clin Microbiol Infect. 2015 Jan;21(1):3-9. DOI: 10.1016/j.cmi.2014.08.018
[5] Rossio R, Franchi C, Ardoino I, Djade CD, Tettamanti M, Pasina L, Salerno F, Marengoni A, Corrao S, Marcucci M, Peyvandi F, Biganzoli EM, Nobili A, Mannucci PM; REPOSI Investigators. Adherence to antibiotic treatment guidelines and outcomes in the hospitalized elderly with different types of pneumonia. Eur J Intern Med. 2015 Jun;26(5):330-7. DOI: 10.1016/j.ejim.2015.04.002
[6] Hepper HJ, Sieber C, Cornel S, Walger P, Peter W, Bahrmann P, Philipp B, Singler K, Katrin S. Infections in the elderly. Crit Care Clin. 2013 Jul;29(3):757-74. DOI: 10.1016/j.ccc.2013.03.016
[7] Ewig S, Höffken G, Kern WV, Rohde G, Flick H, Krause R, Ott S, Bauer T, Dalhoff K, Gatermann S, Kolditz M, Krüger S, Lorenz J, Pletz M, de Roux A, Schaaf B, Schaberg T, Schütte H, Welte T. Behandlung von erwachsenen Patienten mit ambulant erworbener Pneumonie und Prävention – Update 2016 [Management of Adult Community-acquired Pneumonia and Prevention – Update 2016]. Pneumologie. 2016 Mar;70(3):151-200. DOI: 10.1055/s-0042-101873
[8] Böhm K, Tesch-Römer C, Ziese T, editors. Gesundheit und Krankheit im Alter. Berlin: RKI; 2009. (Gesundheitsberichterstattung des Bundes). Available from: https://www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GBEDownloadsB/alter_gesundheit.html
[9] Glaeske G, Trittin C, editors. Weichenstellung: Altern in unserer Gesellschaft. Neue Herausforderungen für das Gesundheitswesen. [Beiträge des 2. Medizinkongresses der Gmünder ErsatzKasse GEK und des Zentrums für Sozialpolitik der Universität Bremen 2007]. St.-Augustin: Asgard; 2008. (GEK-Edition Schriftenreihe zur Gesundheitsanalyse; 62). DOI: 10.4126/FRL01-006401684
[10] Mayer KU, Baltes PB, editors. Die Berliner Altersstudie. Berlin: Akademie Verlag; 1996.
[11] Norman DC. Fever in the elderly. Clin Infect Dis. 2000 Jul;31(1):148-51. DOI: 10.1086/313896
[12] Simonetti AF, Viasus D, Garcia-Vidal C, Carratalà J. Management of community-acquired pneumonia in older adults. Ther Adv Infect Dis. 2014 Feb;2(1):3-16. DOI: 10.1177/2049936113518041
[13] Hortmann M, Singler K, Geier F, Christ M. Erkennen von Infektionen beim älteren Notfallpatienten [Recognition of infections in elderly emergency patients]. Z Gerontol Geriatr. 2015 Oct;48(7):601-7. DOI: 10.1007/s00391-015-0903-2
[14] Nordheim J, Maaz A, Winter MHJ, Kuhlmey A, Hofmann W. Vielnutzung von Krankenversicherungsleistungen im Alter – eine Analyse von Krankenhaus- und Arzneimitteldaten. Z Evid Fortb Qual Gesundheitswesen. 2006;100(8):609-15.
[15] Paffrath U, Schwabe D, editors. Arzneiverordnungsreport (AVR). Berlin: Springer Verlag; 2005.
[16] Glaeske G, Janhsen K. GEK Arzneimittelreport. Asgard: St Augustin; 2005. (Schriftenreihe zur Gesundheitsanalyse; 36). Available from: https://www.barmer.de/blob/38794/69caad9cdc56978154af12bdac7aa874/data/pdf-arzneimittel-report-2005.pdf
[17] Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002 Jan;287(3):337-44. DOI: 10.1001/jama.287.3.337
[18] Kelly JP, Kaufman DW, Kelley K, Rosenberg L, Anderson TE, Mitchell AA. Recent trends in use of herbal and other natural products. Arch Intern Med. 2005 Feb;165(3):281-6. DOI: 10.1001/archinte.165.3.281
[19] Nahin RL, Fitzpatrick AL, Williamson JD, Burke GL, Dekosky ST, Furberg C; GEM Study Investigators. Use of herbal medicine and other dietary supplements in community-dwelling older people: Baseline data from the ginkgo evaluation of memory study. J Am Geriatr Soc. 2006 Nov;54(11):1725-35. DOI: 10.1111/j.1532-5415.2006.00942.x
[20] Bolon M, Weber SG. General Principles of antimicrobial selection. In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, High KP, Asthana A, editors. Hazzard’s Geriatric Medicine and Gerontology. 6th ed. New York, Chicago: Mc Craw Hill Medical; 2009. p. 1517-30.
[21] Veehof LJ, Stewart RE, Meyboom-de Jong B, Haaijer-Ruskamp FM. Adverse drug reactions and polypharmacy in the elderly in general practice. Eur J Clin Pharmacol. 1999 Sep;55(7):533-6. DOI: 10.1007/s002280050669
[22] Nash DB, Koenig JB, Chatterton ML. Why the elderly need individualized phermaceutical care. Philadelphia: Office of Health Policy and Clinical Outcomes / Thomas Jefferson University, April 2000. Available from: https://www.npcnow.org/system/files/research/download/Why-the-Elderly-Need-Individualized-Pharmaceutical-Care.pdf
[23] Thürmann PA, Werner U, Hanke F, Schmiedl S, Drewelow B, Hippius M, et al. Arzneimittelrisiken bei hochbetagten Patienten: Ergebnisse deutscher Studien. In: 31 Interdisziplinäres Forum der Bundesärztekammer „Fortschritt und Fortbildung in der Medizin“; 2007 Jan 11-13; Berlin. Cologne: Deutscher Ärzte-Verlag; 2007. p. 216-24.
[24] Beijer HJ, de Blaey CJ. Hospitalisations caused by adverse drug reactions (ADR): a meta-analysis of observational studies. Pharm World Sci. 2002 Apr;24(2):46-54. DOI: 10.1023/A:1015570104121
[25] Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, Farrar K, Park BK, Breckenridge AM. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004 Jul;329(7456):15-9. DOI: 10.1136/bmj.329.7456.15
[26] Rochon PA, Lane CJ, Bronskill SE, Sykora K, Anderson GM, Mamdani MM, Gurwitz JH, Dhalla IA. Potentially inappropriate prescribing in Canada relative to the US. Drugs Aging. 2004;21(14):939-47. DOI: 10.2165/00002512-200421140-00004
[27] Zhan C, Sangl J, Bierman AS, Miller MR, Friedman B, Wickizer SW, Meyer GS. Potentially inappropriate medication use in the community-dwelling elderly: findings from the 1996 Medical Expenditure Panel Survey. JAMA. 2001 Dec 12;286(22):2823-9. DOI: 10.1001/jama.286.22.2823
[28] Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med. 1991 Sep;151(9):1825-32. DOI: 10.1001/archinte.1991.00400090107019
[29] Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med. 1997 Jul;157(14):1531-6. DOI: 10.1001/archinte.1997.00440350031003
[30] Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003 Dec 8-22;163(22):2716-24. DOI: 10.1001/archinte.163.22.2716
[31] Laroche ML, Charmes JP, Merle L. Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol. 2007 Aug;63(8):725-31. DOI: 10.1007/s00228-007-0324-2
[32] McLeod PJ, Huang AR, Tamblyn RM, Gayton DC. Defining inappropriate practices in prescribing for elderly people: a national consensus panel. CMAJ. 1997 Feb;156(3):385-91.
[33] Hanke F, Szymanski J, Jaehde U, Thürmann PA. Drug-related problems in nursing homes – a prospective study [Abstract 8th Annual Congress of Clinical Pharmacology]. Int J Clin Pharmacol Ther. 2006;44(10):500.
[34] Holt S, Thürmann PA. Erstellung einer Liste potentiell inadäquater Medikation für ältere multimorbide Patienten. In: 7. Deutscher Kongress für Versorgungsforschung des Deutschen Netzwerks für Versorgungsforschung. Köln, 16.-18.10.2008. Düsseldorf: German Medical Science GMS Publishing House; 2008. DocP6.9. Available from: http://www.egms.de/de/meetings/dkvf2008/08dkvf182.shtml
[35] Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010 Aug;107(31-32):543-51. DOI: 10.3238/arztebl.2010.0543
[36] Dormann H, Sonst A, Müller F, Vogler R, Patapovas A, Pfistermeister B, Plank-Kiegele B, Kirchner M, Hartmann N, Bürkle T, Maas R. Adverse drug events in older patients admitted as an emergency: the role of potentially inappropriate medication in elderly people (PRISCUS). Dtsch Arztebl Int. 2013 Mar;110(13):213-9. DOI: 10.3238/arztebl.2013.0213
[37] Girndt M, Trocchi P, Scheidt-Nave C, Markau S, Stang A. The Prevalence of Renal Failure. Results from the German Health Interview and Examination Survey for Adults, 2008-2011 (DEGS1). Dtsch Arztebl Int. 2016 Feb;113(6):85-91. DOI: 10.3238/arztebl.2016.0085
[38] Ferraro S, Pasqualetti S, Carnevale A, Panteghini M. Cystatin C provides a better estimate of the effect of glomerular filtration rate on serum human epididymis protein 4 concentrations. Clin Chem Lab Med. 2016 Oct;54(10):1629-34. DOI: 10.1515/cclm-2015-1272
[39] Colantonio LD, Tanner RM, Warnock DG, Gutiérrez OM, Judd S, Muntner P, Bowling CB. The role of cystatin-C in the confirmation of reduced glomerular filtration rate among the oldest old. Arch Med Sci. 2016 Feb;12(1):55-67. DOI: 10.5114/aoms.2016.57580
[40] Wiggins J, Patel SR. Changes in Kidney Function. In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, High KP, Asthana A, editors. Hazzard’s Geriatric Medicine and Gerontology. 6th ed. New York, Chicago: Mc Craw Hill Medical; 2009. p. 1009-15.
[41] Min L, Galecki A, Mody L. Functional disability and nursing resource use are predictive of antimicrobial resistance in nursing homes. J Am Geriatr Soc. 2015 Apr;63(4):659-66. DOI: 10.1111/jgs.13353
[42] Etherton-Beer CD, Inglis T, Waterer G. Prevalence of oropharyngeal antibiotic-resistant flora among residents of aged care facilities: a pilot study. Respirology. 2015 Oct;20(7):1139-41. DOI: 10.1111/resp.12545
[43] Bolon M, Weber SG. General Principles of antimicrobial selection. In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, High KP, Asthana A, editors. Hazzard’s Geriatric Medicine and Gerontology. 6th ed. New York, Chicago: Mc Craw Hill Medical; 2009. p. 1517-30.
[44] Kollef MH, Sherman G, Ward S, Fraser VJ. Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest. 1999 Feb;115(2):462-74. DOI: 10.1378/chest.115.2.462
[45] Bauer JM, Sieber CC. Frailty: ein neues Syndrom mit hoher Relevanz für den Arzt in einer alternden Gesellschaft. Dtsch Med Wochenschr. 2007;112(2):1-4.
[46] Singler K, Heppner HJ. Besonderheiten des älteren Notfallpatienten. Notfall Rettungsmed. 2012;15(3):255-64. DOI: 10.1007/s10049-012-1591-8
[47] Levy DG, Stergachis A, McFarland LV, Van Vorst K, Graham DJ, Johnson ES, Park BJ, Shatin D, Clouse JC, Elmer GW. Antibiotics and Clostridium difficile diarrhea in the ambulatory care setting. Clin Ther. 2000 Jan;22(1):91-102. DOI: 10.1016/S0149-2918(00)87980-1
[48] Gordon D, Young LR, Reddy S, Bergman C, Young JD. Incidence of Clostridium difficile infection in patients receiving high-risk antibiotics with or without a proton pump inhibitor. J Hosp Infect. 2016 Feb;92(2):173-7. DOI: 10.1016/j.jhin.2015.10.009
[49] Ostrowsky B, Ruiz R, Brown S, Chung P, Koppelman E, van Deusen Lukas C, Guo Y, Jalon H, Sumer Z, Araujo C, Sirtalan I, Brown C, Riska P, Currie B. Lessons learned from implementing Clostridium difficile-focused antibiotic stewardship interventions. Infect Control Hosp Epidemiol. 2014 Oct;35 Suppl 3:S86-95. DOI: 10.1086/677828
[50] Lally L, Mannion L. The potential for antimicrobials to adversely affect mental state. BMJ Case Rep. 2013 Jul 5;2013. pii: bcr2013009659. DOI: 10.1136/bcr-2013-009659
[51] Ben-Chetrit E, Rothstein N, Munter G. Ciprofloxacin-induced psychosis. Antimicrob Agents Chemother. 2013 Aug;57(8):4079. DOI: 10.1128/AAC.00672-13
[52] Mattappalil A, Mergenhagen KA. Neurotoxicity with antimicrobials in the elderly: a review. Clin Ther. 2014 Nov;36(11):1489-511.e4. DOI: 10.1016/j.clinthera.2014.09.020
[53] Sakai Y, Naito T, Arima C, Miura M, Qin L, Hidaka H, Masunaga K, Kakuma T, Watanabe H. Potential drug interaction between warfarin and linezolid. Intern Med. 2015;54(5):459-64. DOI: 10.2169/internalmedicine.54.3146
[54] Lippi G, Favaloro EJ, Mattiuzzi C. Combined administration of antibiotics and direct oral anticoagulants: a renewed indication for laboratory monitoring? Semin Thromb Hemost. 2014 Oct;40(7):756-65. DOI: 10.1055/s-0034-1381233
[55] Lane MA, Zeringue A, McDonald JR. Serious bleeding events due to warfarin and antibiotic co-prescription in a cohort of veterans. Am J Med. 2014 Jul;127(7):657-63.e2. DOI: 10.1016/j.amjmed.2014.01.044
[56] Altena R, van Roon E, Folkeringa R, de Wit H, Hoogendoorn M. Clinical challenges related to novel oral anticoagulants: drug-drug interactions and monitoring. Haematologica. 2014 Feb;99(2):e26-7. DOI: 10.3324/haematol.2013.097287
[57] Clark NP, Delate T, Riggs CS, Witt DM, Hylek EM, Garcia DA, Ageno W, Dentali F, Crowther MA; Warfarin-Associated Research Projects and Other Endeavors Consortium. Warfarin interactions with antibiotics in the ambulatory care setting. JAMA Intern Med. 2014 Mar;174(3):409-16. DOI: 10.1001/jamainternmed.2013.13957
[58] Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007 Dec;5(4):345-51. DOI: 10.1016/j.amjopharm.2007.12.002
[59] Clark DB, Andrus MR, Byrd DC. Drug interactions between linezolid and selective serotonin reuptake inhibitors: case report involving sertraline and review of the literature. Pharmacotherapy. 2006 Feb;26(2):269-76. DOI: 10.1592/phco.26.2.269
[60] Serio RN. Acute delirium associated with combined diphenhydramine and linezolid use. Ann Pharmacother. 2004 Jan;38(1):62-5. DOI: 10.1345/aph.1D018
[61] Lorenz RA, Vandenberg AM, Canepa EA. Serotonergic antidepressants and linezolid: a retrospective chart review and presentation of cases. Int J Psychiatry Med. 2008;38(1):81-90. DOI: 10.2190/PM.38.1.h
[62] Niwa T, Morimoto M, Hirai T, Hata T, Hayashi M, Imagawa Y. Effect of penicillin-based antibiotics, amoxicillin, ampicillin, and piperacillin, on drug-metabolizing activities of human hepatic cytochromes P450. J Toxicol Sci. 2016 Feb;41(1):143-6. DOI: 10.2131/jts.41.143
[63] Bolhuis MS, Panday PN, Pranger AD, Kosterink JG, Alffenaar JW. Pharmacokinetic drug interactions of antimicrobial drugs: a systematic review on oxazolidinones, rifamycines, macrolides, fluoroquinolones, and Beta-lactams. Pharmaceutics. 2011 Nov 18;3(4):865-913. DOI: 10.3390/pharmaceutics3040865
[64] Niedrig D, Maechler S, Hoppe L, Corti N, Kovari H, Russmann S. Drug safety of macrolide and quinolone antibiotics in a tertiary care hospital: administration of interacting co-medication and QT prolongation. Eur J Clin Pharmacol. 2016 Jul;72(7):859-67. DOI: 10.1007/s00228-016-2043-z
[65] Frommeyer G, Fischer C, Lange PS, Leitz P, Fehr M, Bogossian H, Milberg P, Eckardt L. Divergent electrophysiologic profile of fluconazole and voriconazole in an experimental whole-heart model of proarrhythmia. Eur J Pharmacol. 2016 Apr;776:185-90. DOI: 10.1016/j.ejphar.2016.02.051
[66] Tholakanahalli VN, Potti A, Hanley JF, Merliss AD. Fluconazole-induced torsade de pointes. Ann Pharmacother. 2001 Apr;35(4):432-4. DOI: 10.1345/aph.10210
[67] Paparella M, Martina V, Rizzo MA, Gallieni M. What every doctor should know about drug safety in patients with chronic kidney disease. Contrib Nephrol. 2015;184:24-50. DOI: 10.1159/000365821
[68] Antoniou T, Gomes T, Juurlink DN, Loutfy MR, Glazier RH, Mamdani MM. Trimethoprim-sulfamethoxazole-induced hyperkalemia in patients receiving inhibitors of the renin-angiotensin system: a population-based study. Arch Intern Med. 2010 Jun;170(12):1045-9. DOI: 10.1001/archinternmed.2010.142
[69] Mörike K, Schwab M, Klotz U. Use of aminoglycosides in elderly patients. Pharmacokinetic and clinical considerations. Drugs Aging. 1997 Apr;10(4):259-77. DOI: 10.2165/00002512-199710040-00003
[70] Bruniera FR, Ferreira FM, Saviolli LR, Bacci MR, Feder D, da Luz Gonçalves Pedreira M, Sorgini Peterlini MA, Azzalis LA, Campos Junqueira VB, Fonseca FL. The use of vancomycin with its therapeutic and adverse effects: a review. Eur Rev Med Pharmacol Sci. 2015 Feb;19(4):694-700.
[71] Shields RK, Martello JL, Potoski BA. Is vancomycin ototoxicity a significant risk? Antimicrob Agents Chemother. 2009 Oct;53(10):4572; author reply 4572-3. DOI: 10.1128/AAC.00537-09
[72] Thomas JA, Burns RA. Important drug-nutrient interactions in the elderly. Drugs Aging. 1998 Sep;13(3):199-209. DOI: 10.2165/00002512-199813030-00003
[73] Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991 Jun;148(6):705-13. DOI: 10.1176/ajp.148.6.705




