[The Munich Declaration – Key Points for the Establishment Teaching in the New Cross-disciplinary Area 13: Palliative Medicine at German Faculties]
Isabel Dietz 1Frank Elsner 2
Christine Schiessl 3
Gian Domenico Borasio 4
1 Department of Anaesthesiologie I, University Witten/Herdecke, Helios Clinik Wuppertal, Wuppertal, Germany
2 RWTH University Aachen, University Hospital, Department for Palliative Medicine, Aachen, Germany
3 University Hospital of Cologne, Centre for Palliative Medicine, Cologne, Germany
4 CHUV, Chair of Palliative Medicine, Lausanne, Switzerland
Introduction
The development of the teaching of palliative medicine at the medical faculties in Germany and the discussion about the inclusion of palliative care as a subject into the Medical Licensure Act follows a lengthy process [1].
Various publications repeatedly drew attention to existing skills gaps among young physicians and medical students in dealing with terminally ill and dying patients due to inadequate teaching in the field of palliative medicine in Germany [2], [3], [4], [5]. However, the Medical Licensure Act (Appendix 15 to § 29 Para 3 Sentence 2) previously only listed the subject as optional but not mandatory examination material for the second part of the medical examinations towards the end of medical studies. Thus the implementation and delivery of palliative care training remained was left to the commitment of individual universities.
Against this backdrop, the development of appropriate structures in Germany was slow. In 2009 only five of 36 medical faculties in Germany had occupied chairs for palliative care, at only 6 universities were compulsory courses in palliative medicine offered, of which only half concluded the course with an exam counting towards the degree [1].
As of 5 August 2009, palliative medicine was integrated into the Medical Licensure Act as the 13th cross-disciplinary area (QB 13) [6]. This means that from 2013 onwards, all medical faculties in Germany will require students to pass relevant examinations in specialist palliative care in order to be admitted to the Practical Year.
The fact that by now 34 faculties teach palliative care content - albeit with significant qualitative and quantitative differences - illustrates that in principle both access to qualified lecturers in palliative care and a broad willingness to establish teaching structures exist. So far, only those few faculties with chairs in palliative care can offer high-quality structured training, as described by Alt-Epping et al. for teaching palliative care at the University of Göttingen [7].
To ideally and appropriately facilitate the introduction of palliative care courses which are now legally required into general university curricula at less well-equipped faculties, the chairs of the universities of Aachen, Cologne and LMU Munich in cooperation with the German Society for Palliative Medicine (DGP) and the National Association of Medical Students in Germany (bvmd) organised a workshop on this topic.
Lecturers and students from 25 medical schools met on the 2
The central point of discussion at the event was the question of how high-quality and comparable teaching in palliative care can be established across Germany within the short timeframe and in spite of differences in resources and settings at the various faculties. Common goals and guidelines were recorded in the form of the Munich Declaration and will be presented in the following.
The Munich Declaration
Structural Quality in Palliative Teaching
Extent and Content
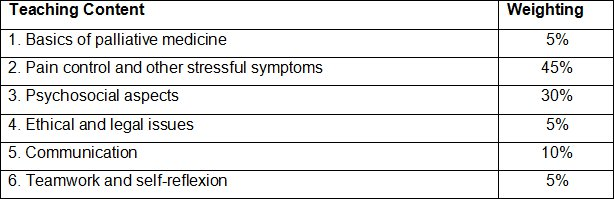
In line with European developments and the recommendations of the German Society for Palliative Medicine, the scope of the new QB 13 Palliative Medicine should be 40 teaching units (TU) of 45 minutes. It should be examined to what extent individual TU are already covered in other areas of the curriculum or how they may be offered in cooperation with other disciplines (medical psychology, medical law, medical ethics, psychosomatics/psychotherapy, anaesthesia/pain management, internal medicine/oncology, general practice, etc.). The target should not fall short of 20 obligatory hours of face to face teaching by a tutor working full-time in palliative care. The teaching content should correspond to the “Curriculum for the Teaching of Palliative Care” by the DGP (see Table 1 [Tab. 1]). Superficial repetition of teaching content from other subjects should be avoided [8].
Teaching Staff
One member of the teaching staff responsible for the subject of palliative medicine is to be designated by the respective faculty. This must be an active full-time palliative care specialist, ideally the holder of an independent chair of palliative medicine at the faculty level. The creation of dependent professorships does not meet the needs of the subject of palliative care in research and teaching [9]. If the faculty does not have such structures, alternatively, an external specialist who is working actively and full-time in palliative care, for example the head of a palliative care unit of an associated teaching hospital or a recognized SAPV team can be appointed as the responsible member of the teaching staff. Additional lecturers should also be full-time professionals working in palliative care as a rule. The inclusion of lecturers who are not physicians has proven successful in the areas of psychosocial and spiritual palliative care and is therefore strongly recommended, especially as physicians generally indicate a distinct lack of palliative training as regards their psychosocial competences [9]. A qualification in palliative care teaching is desirable for a multi-professional teaching staff [10], [11].
Process Quality in Palliative Medical Teaching
Teaching Format
Experience has shown that knowledge, skills and attitudes in palliative care are best taught in smaller groups of students, as this format promotes intensive exchange of ideas and the opportunity for self-reflection. Of the 20 obligatory hours in QB 13, at least half should therefore be conducted in seminars with a maximum of 20 students or smaller groups. Monitoring attendance is essential and missed units must be re-taken.
Experience has also shown that bedside teaching, which is the desired format and the didactic target, is usually difficult to achieve through the (low) number of existing palliative beds and student numbers. The inclusion of palliative care structures in the outpatient domain (for example SOPC teams) into the teaching concepts is highly recommended as this enables palliative medical training outside palliative care wards (for example in the home, in nursing homes or inpatient hospices). Offers for additional training, including ward routines, elective seminars (for example on topics such as palliative care for children, end of life decisions, etc.) and - in the presence of a palliative care unit - offering an optional three month course in palliative care during the Practical Year are appropriate ways to expand the range of courses offered for particularly interested students. In addition, simulations such as role playing and contact with actor patients can also be used for teaching communication and social competences.
Quality Control
The quality of the results must be documented through periodic evaluations. Both an evaluation of the lecturers and the course content and exams should be required. All evaluation results should be made available to the responsible member of the teaching staff so that appropriate conclusions can be drawn.
Finance
The subject of palliative care should benefit from the same financial resources available to other compulsory subjects of a comparable size in the medical curriculum in accordance with its importance as a new compulsory curricular subject and examination subject, as only this will ensure high-quality teaching. Different ways of calculating financial models exist at medical faculties (for example in terms of performance-oriented allocation of funds - LOM) which should be similarly applied to palliative care as a subject. The innovative character of the enriching, but challenging in terms of its organisational structure, multi-professional nature of palliative care should be taken into account and the establishment of appropriate educational structures should be promoted. In determining the share of funding for the new QB 13 the number of hours in the overall curriculum should be used as the primary benchmark and then set in relation to the total teaching budget at the respective faculty. Other factors which may be considered are quality issues assessed through student evaluations and, during the first few years, the objective need for seed funding for the initial establishment of structures in the teaching of palliative care.
Discussion
The introduction of the new QB 13 represents a decisive course change for the future of palliative care in Germany. By facilitating comprehensive palliative care education of future physicians, a sustainable improvement in general palliative care will be achievable. This requires high-quality of teaching of compulsory modules in order to make the next generation of doctors engage with the subject and to give them a basic understanding of best-practice in supporting terminal patients. As the necessary staffing and structural conditions currently are known not to be present at all medical faculties in Germany, there is now the need to support those universities appropriately. Our workshop from July last year should be seen as a first step. Some important issues, such as form, content and design of exams or defining learning objectives could not be addressed in depth at the workshop and should be dealt with at similar events in the future.
The large number of participants at the first workshop on the one hand reflects the need for training and information in the areas of curriculum development and teaching but also the interest and involvement of those working in the teaching of palliative care. As comprehensive, high-quality teaching of students cannot be ensured by dedicated individuals, it is now up to the medical faculties to provide adequate support in the construction phase. The targets, requests and guidelines referred to in this paper are meant to give help and guidance.
As close collaboration with students has proven fruitful in the past, continued joint development of compulsory teaching should be aimed for [12].
Even if our goal is to teach 40 hours of palliative content in total in accordance with the requirements of the European Association for Palliative Care (EAPC), one must be aware, however, that this goal has not been achieved in neighbouring European countries either [13], [14]. This should not lead to flagging efforts but rather serve as an incentive to achieve the common goal step by step through comparison and exchange with our neighbours.
Competing interests
The authors declare that they have no competing interests.
References
[1] Laske A, Ilse B, Nauck F, Elsner F. Palliativmedizinische Lehre in Deutschland – Bestandsaufnahme an den medizinischen Fakultäten 2009. Z Palliativmed. 2010;11:18-25. http://dx.doi.org/10.1055/s-0029-1223482[2] Clemens KE, Klein E, Jaspers B, Klaschik E. Attitudes toward active euthanasia among medical students at two German universities. Support Care Cancer. 2008;16(6):539-545. http://dx.doi.org/10.1007/s00520-008-0427-z
[3] Klaschik E. Palliative medicine--a requirement in clinical practice, education and research. Krankenpfl J. 2000;38(1-2):20-22.
[4] Klaschik E, Nauck F. Palliativmedizin. Defizite in der studentischen Ausbildung. Dtsch Arztebl. 2002;99:A1286–1288.
[5] Ostgathe C, Nauck F, Klaschik E, Dickerson ED. German medical education in pain therapy and palliative medicine: a comparison of British, Canadian, and United States models. J Pain Symptom Manage. 2002;24(1):13-15. http://dx.doi.org/10.1016/S0885-3924(02)00427-X
[6] Bundestag D. Gesetzentwurf der Fraktionen CDU/CSU und SPD. Entwurf eines Gesetzes zur Regelung des Assistenzpflegebedarfs im Krankenhaus. Berlin: Dtsch Bundestag; 2009. Volume Drucksache 16/12855.
[7] Alt-Epping B, Jung W, Simmenroth-Nayda A, Russo SG, Vormfelde SV, Nauck F. Implementierung des Querschnittsfachs Palliativmedizin (Q13) vor dem Hintergrund der neuen gesetzlichen Rahmenbedingungen am Beispiel der Universitätsmedizin Göttingen. GMS Z Med Ausbild. 2010;27(5):Doc67. DOI: 10.3205/zma000704
[8] Deutschen Gesellschaft für Palliativmedizin e.V. Curriculum: Grundlagen der Palliativmedizin. Gegenstandskatalog und Lernziele für Studierende der Medizin. 2. überarbeitete Fassung. Berlin: Deutsche Gesellschaft für Palliativmedizin; 2009. Zugänglich unter/available from: http://www.dgpalliativmedizin.de/images/stories/pdf/ag/090810%20AG%20AFW%20Curriculum%20Studierende%20Elsner%20Stand%20090810.pdf
[9] Deutschen Gesellschaft für Palliativmedizin e.V. Stellungnahme der Deutschen Gesellschaft für Palliativmedizin (DGP) zur Einrichtung von Lehrstühlen für Palliativmedizin an den medizinischen Fakultäten vom 10.2.2009. Berlin: Deutsche Gesellschaft für Palliativmedizin; 2009. Zugänglich unter/available from: http://www.dgpalliativmedizin.de/images/stories/pdf/sn/SN%20090210%20DGP%20Lehrstuehle.pdf
[10] Wasner M, Roser T, Fittkau-Tönnesmann B, Borasio GD. Palliativmedizin im Studium: Spiritualität und psychosoziale Begleitung als wichtige Lehrinhalte. Dtsch Ärztebl. 2008;105:A-674-A676.
[11] Becker G, Momm F, Gigl A, Wagner B, Baumgartner J. Competency and educational needs in palliative care. Wien Klin Wochenschr. 2007;119(3-4):112-116. http://dx.doi.org/10.1007/s00508-006-0724-9
[12] Bundesvertretung der Medizinstudierenden in Deutschland. Leitfaden der AG Palliativmedizin der bvmd. Bonn: Bundesvertretung der Medizinstudiernden in Deutschland; 2010. Zugänglich unter/available from: http://bvmd.de/fileadmin/PALLIATIV/Leitfaden_Palliativmedizin_bvmd_20101901.pdf
[13] Gibbins J, McCoubrie R, Maher J, Wee B, Forbes K. Recognizing that it is part and parcel of what they do: teaching palliative care to medical students in the UK. Palliat Med. 2010;24(3):299-305. http://dx.doi.org/10.1177/0269216309356029
[14] Pereira J, Pautex S, Cantin B, Gudat H, Zaugg K, Eychmuller S, Zulian G. Palliative care education in Swiss undergraduate medical curricula: a case of too little, too early. Palliat Med. 2008;22(6):730-735. http://dx.doi.org/10.1177/0269216308094560




