[Conflicts of interest in medical school: Missing Policies and high need for student information at most German Universities]
Klaus Lieb 1Cora Koch 2
1 University Medical Center Mainz, Department of Psychiatry and Psychotherapy, Mainz, Germany
2 Westfälische Wilhelms-University of Münster, Münster, Germany
Abstract
Objectives: Medical students interact with pharmaceutical representatives already during medical school. The goal of this study was to find out:
- Do policies exist at German medical faculties that govern the interactions between medical students and pharmaceutical representatives, do schools offer courses on the subject and do students attend these courses? And
- What are the attitudes of medical students concerning the role of pharmaceutical companies in medical teaching?
Methods: All 36 German medical faculty deans and 1,151 medical students at eight German universities were asked to complete a questionnaire of 4 and 7 questions, respectively, regarding the above mentioned topics.
Results: 30 (83,3%) deans and 1,038 (90.3%) medical students filled in the questionnaire, respectively. According to the deans' answers, only one school had a policy concerning conflicts of interest and one had a policy governing the interactions between medical students and industry. 8 (26.7%) deans showed an interest in constructing a policy or educational an activity on this subject. 149 (14,4%) students had participated in an activity that focussed the subject of conflicts of interest and 779 (77,8%) wanted more education on the subject. 701 (73,4%) were opposed to an improvement of medical studies through financial support by pharmaceutical companies, whereas 216 (21,9%) were of the opinion that students should not meet with pharmaceutical representatives.
Conclusions: Unlike in other countries, like the US, most German medical faculties do not have policies that govern the interactions between medical students and pharmaceutical companies. Since most students want to be taught more about these interactions, the implementation of respective policies and lectures would be desirable.
Keywords
Conflict of interest, pharmaceutical industry, independence, medical training, teaching
Introduction
International studies have shown that medical students frequently come into contact with representatives of pharmaceutical companies (PCs) [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11]. Contact rates of between 74 and 100% have been found for students of clinical medicine [3], [4]. Our survey of German medical students [12] also showed high rates of contact and similarly varied types of contact, as had already been shown by earlier studies conducted among doctors [13]: inter alia, they received gifts, took part in sponsored events or were treated to sponsored meals [1], [2].
Various studies have suggested that the contact between doctors and representatives of PCs can lead to changes in prescription behaviour, as increased levels of contact with pharmaceutical representatives are associated with higher prescription costs and a reduction in the quality of prescriptions [14]. Even small gifts can have an effect, which is often not even noticed by the recipients themselves [15]. It has also been shown that promotional gifts can influence the perception that students have of certain medicinal products [6].
In the USA, most medical faculties have instituted policies to deal with conflicts of interest arising from contact with PCs, which also serve to regulate contact between students and PCs [16], [
To date, there has been no data on this topic for Germany. The objective of this study was thus to ascertain whether medical faculties in Germany have policies on conflicts of interest, whether they offer any lecture courses on the topic, and whether and to what extent medical students are aware of these policies and lecture courses. We also investigated how students perceive the role of PCs in medical training.
Methods
All student affairs' deans of the 36 medical faculties in Germany were written to on 29.11.2011 and were requested to respond to a questionnaire. As not all of the deans replied to our request immediately, certain deans had to be written to again. This lasted until 22.03.2012. These questionnaires contained 4 questions, of which two asked about the existence of a policy which focused on the topic of “conflicts of interest” and/or about the existence of a policy which dealt with and, if applicable, regulated the interactions between medical students and the industry. With the 3
The student questionnaire was a German translation of the questionnaire developed by Sierles et al. [1], the questionnaire submitted to the deans took questions from the questionnaire published by Sierles et al. in 2009 [17]. The results are presented both as percentages of the responses given to the listed questions and in absolute numbers. The descriptive statistical analysis was carried out using SPSS 20.0 software.
Results
Samples
Of the 36 deans contacted, 30 (83,3%) completed the questionnaire and returned it no later than 10.05.2012. The deans of the following universities did not return the questionnaire: Berlin, Heidelberg, Kiel, Leipzig, Düsseldorf and Tübingen. Of the 1,151 medical students surveyed 90.3% (n=1,039) returned the completed questionnaire anonymously (Aachen n=35, Dresden n=165, Freiburg n=305, Gießen n=119, Göttingen n=92, Jena n=167, Cologne n=129, Münster n=139). One questionnaire of a foreign Erasmus exchange student was excluded, which meant that 1,038 questionnaires were evaluated. Demographic data from the medical student-sample are given in Lieb and Koch [12].
Responses from the deans regarding policies and lectures
According to the information given by the deans, there is at respectively only one (3.3%) medical faculty a policy on the topic of conflicts of interest or a policy regulating interactions between medical students and the industry. The dean of Aachen University declared that it is not permitted for companies to make contact with medical students in the Aachen University Hospital and that presentations are only permitted after consultation with the faculty staff and can be disallowed by the dean. The dean of the medical faculty in Dresden stated that there is a policy on conflicts of interest, but he gave no further information.
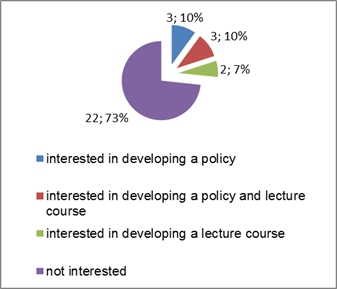
6 faculties expressed interest in formulating a policy (see Figure 1 [Fig. 1]) and 5 (16.7%) are currently planning such a policy. 6 medical faculties stated that they offered a lecture on the topic of conflicts of interest. Information is communicated as part of the following lecture courses: Medical Ethics (Bonn, Erlangen, Homburg), Pharmacoeconomics (Gießen), General Medicine (Göttingen), Pharmacology (Frankfurt) and Clinical Studies (Cologne). 5 (16.7%) of the deans expressed interest in preparing a lecture on this topic (see Figure 1 [Fig. 1]) and 2 (6.7%) deans stated that such a lecture is currently being planned.
Student participation in lecture courses and attitudes to the role of PCs in medical training
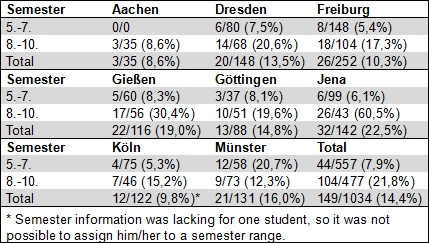
149 (14.4%) of medical students had already taken part in a class which focused on the topic of conflicts of interest. Table 1 [Tab. 1] shows the distribution according to university and semester. 141 responded to the question about whether the lecture was elective or required: for 15 (10.6%) medical students it was required, for 126 (89.4%) it was elective. At 3 universities, which offered a lecture and at which the students were surveyed, of the students who should have already attended the corresponding lectures only a low proportion (20% for University 5, 30% for University 4, 15% for University 7) stated that they had already had a lecture on this topic.
899 (87.8%) of students did not know if their university had a policy regulating the interaction between medical students and the industry (see Table 2 [Tab. 2]). Of the 8 universities at which the student survey was carried out, only Aachen and Dresden mentioned the existence of a policy. Of the 34 students surveyed in Aachen, 25 (73.5%) knew nothing of this policy, 4 (11.8%) knew that there was a policy but did not know what it was, one (2.9%) student thought that there was no policy or that there was a policy which did not limit any interactions, while three (8.8%) gave the correct information, namely that a policy does exist which places a limit on such contacts. In Dresden, 135 (90.6%) knew nothing of this policy, 13 (8.7%) knew that there was a policy but did not know what it was, and 1 (0.7%) student thought that there was no policy, while none of the 149 students in Dresden who responded to this question were correctly informed about the existence of this policy.
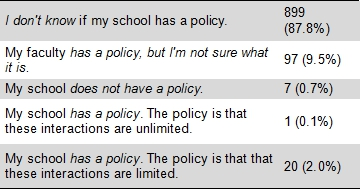
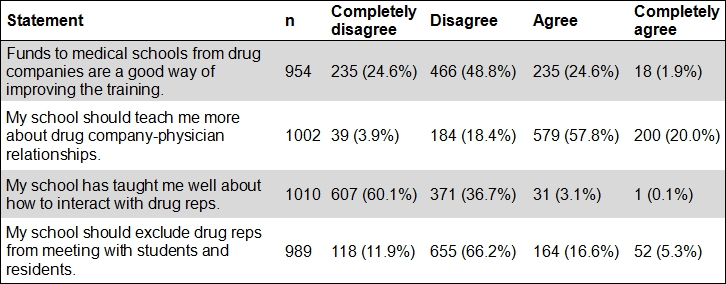
Table 3 [Tab. 3] summarises the medical students’ responses about the role of PCs in medical training. 779 (77.8%) students would like to be taught more about relations with PCs. Similarly, 978 (96.8%) of students expressed the opinion that they were not sufficiently prepared to deal with representatives of PCs. 701 (73.4%) opposed the improvement of medical training through the financial support of PCs, whereas 216 (21.9%) were of the opinion that students should not meet with representatives of PCs.
Discussion
Our survey has shown that in Germany only two universities have instituted policies which regulate the interactions between medical students and PCs. This stands in sharp contrast to the USA where, according to a survey conducted by the American Medical Students' Association (AMSA), 144 to 158 medical faculties have policies dealing with conflicts of interest which also mention interactions between students and PCs [
It was a surprise to us that the universities’ interest in formulating corresponding policies for both students and teaching staff was relatively low: Only 6 out of 30 universities without any policies stated that they were interested in formulating one. On the one hand, this would seem to suggest a lack of awareness of the problem amongst the deans. Until now, there has also been no data available about how students interact with PCs in Germany. Ours was the first survey [12] to show clearly that medical students in Germany also come into close contact with PCs. On the other hand, this lack of interest on the part of the deans may also be because they view such policies as being ineffective instruments of control. In fact, a study recently published in the USA showed that policies do little to change the behaviour of medical students [11]. While on the other hand, another study concluded that the disclosure of conflicts of interests by lecturers had a considerable influence on the students’ attitudes [18].
At the two universities that stated that they had a policy on interactions between students and PCs, we were able to survey approximately 185 students about their knowledge of these policies. This revealed that only very few students were aware of the policies: overall, only 3 students were correctly informed about the policies. This highlights the necessity that universities must also make the students aware of the policies that they do introduce. If there is no awareness or implementation of a policy it can, of course, achieve nothing.
When the students were questioned about the role of PCs in medical training it was noticeable that, on the one hand, approximately ¾ of students were of the opinion that the financing of medical training by PCs was not a good way of improving training, at the same time, however, ¾ of students were of the opinion that universities should not forbid interactions between pharmaceutical representatives and medical students. It is possible that the students objectively view any influence of PCs in medical training as being problematic, but subjectively they feel themselves to be in a position to be able to control their interactions with the pharmaceutical representatives in such a way that they are not influenced. This is a typical constellation of what is frequently described as a 'blind spot', i.e. the lack of awareness of one’s own suggestibility, even though the danger of being influenced is seen objectively. This “blind spot” has been shown repeatedly both amongst students [1], [12] and doctors [13], [19], [20]. On the other hand, this contrast can also be interpreted simply in that, in line with a graded degree of risk of being influenced, the majority of students actually want to have contact with representatives of pharmaceutical companies, because they feel that they can learn something from them and that they can control such contacts. However, they oppose the direct financial support of medical training and thus the possibility of being directly – and unnoticed by the students - influenced. Corresponding to the result that only six of the surveyed universities stated that they offered a course on the topic of conflicts of interests and that only approximately 14% of students had already taken part in a lecture course, nearly all the students (96.8%) felt themselves to have been poorly taught in this regard, and that most of them would have liked correspondingly more instruction on interactions between students and PCs. In our opinion, this desire of the students should motivate the medical faculties to offer corresponding lectures or other teaching sessions so that they do not only take action because of external pressure, as happened in the USA through AMSA. Such lectures or seminars should be compulsory in order to reach all students because – as our results have shown – only a small proportion of students attend such teaching sessions if they are only offered on a voluntary basis. However, one must bear in mind that the question of what the appropriate teaching sessions are and how one might best measure their effectiveness has also been a matter of critical discussion internationally, and there is no unanimous opinion on the topic.
Our survey was essentially limited in that we received no response from 6 deans despite repeated requests and thus no overall view of the situation in Germany could be produced. Furthermore, we did not carry out any separate enquiries (e.g. on-line) in order to verify the statements made by the deans. Whereas it must be assumed that the deans are at least likely to be aware of any policies in their faculties, it is probable that they do not know about all teaching sessions on the topic of conflicts of interest that are offered at their universities. We know, for example, that Berlin’s Charité University Hospital (which unfortunately did not take part in our survey) offers an elective course on marketing in the pharmaceutical industry, which is very well attended by the students [21], and at the University Hospital Mainz a lecture on the topic of conflicts of interest is offered as part of the main psychiatry and psychotherapy course, of which the dean was unaware.
Conclusions
In contrast to other countries, such as the USA, there are no policies in place in German medical faculties regulating the interaction of medical students with pharmaceutical companies, apart from a very few exceptions. As the majority of students would like to have more information about these interactions and as changes to prescription behaviour amongst doctors caused by contacts with PCs have been described many times, we consider the establishment of corresponding lecture courses and/or policies as sensible. These should improve the problematic lack of awaress about students' interactions with PCs and also induce behaviour changes, e.g. by offering seminars including role-playing sessions with simulated representatives of pharmaceutical companies. Such measures must still in large part be developed and implemented, and their impact on the later behaviour of doctors and their prescription behaviour must be carefully evaluated.
Note
This paper contains extended passages from the dissertation by Cora Koch.
Acknowledgement
We would like to thank Dr. R. Sierles for the permission to use his two questionnaires [1], [17] as well as the deans and students who took part for their support and cooperation.
Competing interests
The authors declare that they have no competing interests.
References
[1] Sierles FS, Brodkey AC, Cleary LM, McCurdy FA, Mintz M, Frank J, Lynn DJ, Chao J, Morgenstern BZ, Shore W, Woodard JL. Medical students' exposure to and attitudes about drug company interactions: a national survey. JAMA. 2005;294(9):1034–1042. DOI: 10.1001/jama.294.9.1034[2] Austad KE, Avorn J, Kesselheim AS. Medical Students' Exposure to and Attitudes about the Pharmaceutical Industry: A Systematic Review. PLoS Med. 2011;8:e1001037. DOI: 10.1371/journal.pmed.1001037
[3] Lea D, Spigset O, Slørdal L. Norwegian medical students' attitudes towards the pharmaceutical industry. Eur J Clin Pharmacol. 2010;66(7):727–733. DOI: 10.1007/s00228-010-0805-6
[4] Wilkes MS, Hoffman JR. An innovative approach to educating medical students about pharmaceutical promotion. Acad Med. 2001;76(12):1271–1277. DOI: 10.1097/00001888-200112000-00026
[5] Wofford JL, Ohl CA. Teaching appropriate interactions with pharmaceutical company representatives: The impact of an innovative workshop on student attitudes. BMC Med Educ. 2005;5:5. DOI: 10.1186/1472-6920-5-5
[6] Grande D, Frosch DL, Perkins AW, Kahn BE. Effect of exposure to small pharmaceutical promotional items on treatment preferences. Arch Intern Med. 2009;169(9):887. DOI: 10.1001/archinternmed.2009.64
[7] Hyman PL, Hochman ME, Shaw JG, Steinman MA. Attitudes of preclinical and clinical medical students toward interactions with the pharmaceutical industry. Acad Med. 2007;82(1):94–99. DOI: 10.1097/01.ACM.0000249907.88740.ef
[8] Monaghan MS, Galt KA, Turner PD, Houghton BL, Rich EC, Markert RJ, Bergman-Evans B. Student understanding of the relationship between the health professions and the pharmaceutical industry. Teach Learn Med. 2003;15(1):14–20. DOI: 10.1207/S15328015TLM1501_04
[9] Sandberg WS, Carlos R, Sandberg EH, Roizen MF. The effect of educational gifts from pharmaceutical firms on medical students' recall of company names or products. Acad Med. 1997;72(10):916–918. DOI: 10.1097/00001888-199710000-00018
[10] Vuorenkoski L, Valta M, Helve O. Effect of legislative changes in drug promotion on medical students: questionnaire survey. Med Educ. 2008;42(12):1172–1177. DOI: 10.1111/j.1365-2923.2008.03169.x
[11] Austad KE, Avorn J, Franklin JM, Kowal MK, Campbell EG, Kesselheim AS. Changing Interactions Between Physician Trainees and the Pharmaceutical Industry: A National Survey. J Gen Intern Med. 2013;28(8):1064–1071. DOI: 10.1007/s11606-013-2361-0
[12] Lieb K, Koch C. Einstellungen und Kontakte von Medizinstudierenden zur Pharmazeutischen Industrie: eine Befragung an 8 Universitätskliniken. Dtsch Arztebl Int. (im Druck)
[13] Lieb K, Brandtönies S. A survey of german physicians in private practice about contacts with pharmaceutical sales representatives. Dtsch Arztebl Int. 2010;107(22):392–398.
[14] Spurling GK, Mansfield PR, Montgomery BD, Lexchin J, Doust J, Othman N, Vitry AI. Information from pharmaceutical companies and the quality, quantity, and cost of physicians' prescribing: a systematic review. PLoS Med. 2010;7(10):e1000352.
[15] Katz D, Caplan AL, Merz JF. All gifts large and small: toward an understanding of the ethics of pharmaceutical industry gift-giving. Am J Bioeth. 2003;3(3):39–46. DOI: 10.1162/15265160360706552
[16] Chimonas S, Patterson L, Raveis VH, Rothman DJ. Managing conflicts of interest in clinical care: a national survey of policies at U.S. medical schools. Acad Med. 2011;86(3):293–299. DOI: 10.1097/ACM.0b013e3182087156
[17] Sierles F, Brodkey A, Cleary L, McCurdy FA, Mintz M, Frank J, Lynn DJ, Chao J, Morgenstern B, Shore W, Woodard J. Relationships between drug company representatives and medical students: medical school policies and attitudes of student affairs deans and third-year medical students. Acad Psychiatry. 2009;33(6):478–483. DOI: 10.1176/appi.ap.33.6.478
[18] Kim A, Mumm LA, Korenstein D. Routine conflict of interest disclosure by preclinical lecturers and medical students' attitudes toward the pharmaceutical and device industries. JAMA. 2012;308(21):2187–2189. DOI: 10.1001/jama.2012.25315
[19] Pronin E, Gilovich T, Ross L. Objectivity in the Eye of the Beholder: Divergent Perceptions of Bias in Self Versus Others. Psychol Rev. 2004;111(3):781–799. DOI: 10.1037/0033-295X.111.3.781
[20] Steinman MA, Shlipak MG, McPhee SJ. Of principles and pens: attitudes and practices of medicine housestaff toward pharmaceutical industry promotions. Am J Med. 2001;110(7):551–557. DOI: 10.1016/S0002-9343(01)00660-X
[21] Erb S. Medizinstudium: Verdächtige Geschenke. Hamburg: Die Zeit; 2012. Zugänglich unter/available from: http://www.zeit.de/2012/13/C-Medizin




