The development of quality of life and hearing ability of adult cochlear implant users in the course of outpatient cochlear implant follow-up therapy
Dennis Metzeld 1Yvonne Seebens 1
Silke Helbig 1,2
1 Cochlear Implant Centre Rhein-Main, Friedberg, Germany
2 Goethe University Frankfurt, University Hospital, ENT-Department, Clinic for Otorhinolaryngology, Frankfurt am Main, Germany
Abstract
Research question: The increase in hearing ability of postlingually deafened patients with cochlear implants (CI) is usually measured using various audiometric tests. In addition, a variety of different subjective measures of patients’ hearing-related and general quality of life (QoL) are also used. Only a few studies deal with the development in the course of the frequently required inpatient or outpatient hearing rehabilitation. The aim of the present study was to measure the development of adult CI patients in the course of outpatient follow-up therapy.
Methods: 58 patients between the ages of 14 and 84 were tested. The measurements using the Freiburg and Oldenburg Sentence (OLSA) Tests and the Nijmegen Cochlear Implant Questionnaire (NCIQ) were taken at the beginning and end of each rehabilitation phase of follow-up therapy.
Results: In all subcategories of the NCIQ and in the overall score, as well as in most audiological measurements, there are significant improvements with small to medium effect sizes over the course of a rehabilitation phase. Patients who had lower scores at the beginning of the rehabilitation phase improved in particular. The improvements are independent of the duration of the rehabilitation phase. At the beginning of the rehabilitation phase, there are significant correlations in the OLSA with the subscales of the NCIQ that are closer to hearing, but only at the end of the rehabilitation phase with the scales that characterize the psychosocial satisfaction of the patients.
Conclusions: In particular, patients with a poorer starting position at the beginning of the rehabilitation phase appear to benefit from outpatient follow-up therapy both in terms of objective measurements and in terms of their subjectively perceived quality of life. The gains in both areas do not seem to develop at the same speed: it is possible that the improved hearing ability must first prove itself in everyday life in order to lead to a higher subjectively perceived quality of life in the long term.
Research question
Hearing tests such as the Oldenburg Sentence Test (OLSA) or the Freiburg mono- and multisyllabic speech test are usually used to check improved hearing ability after CI fitting. However, despite good results in these tests, patients often perceive limitations in everyday communication and in their hearing-related psychosocial situation. The correlations between the audiological measurements on the one hand and the results of the QoL questionnaires on the other are rather low in most studies [1], [2]. Therefore, in parallel to the audiological measurement data, numerous studies also use a variety of different subjective measurement methods for patients’ hearing-related and general quality of life (QoL) [3]. In the case of hearing-related QoL questionnaires usually show improvements, whereas the results of questionnaire instruments for general QoL are often less clear [1]. Most studies focus on comparing the results of patients before and after implantation. Only a few studies look at the development over the course of inpatient or outpatient hearing rehabilitation.
Several studies have used various personality variables, cognitive performance and socio-demographic data of patients to try to predict the gain in patients’ quality of life as a result of CI fitting, with little success to date [2], [4], [5].
The aim of the present study was to measure the development of adult CI patients over the course of outpatient follow-up therapy. To this end, audiological measurements and the Nijmegen Cochlear Implant Questionnaire (NCIQ) [6] in the German translation of Hirschfelder et al. [5] were compared at the beginning and end of a rehabilitation phase. The NCIQ is also recommended in the S2K Guidelines for the Cochlear Implant treatment [7]. The questionnaire is directly hearing related, and comprises three functional and three psychosocial subscales. The following questions were to be answered:
- Are there significant improvements in NCIQ and audiometric tests within a rehabilitation phase?
- Are the measurements of the variables at T1 and/or T2 related?
- Are there definable groups that show particular improvement?
Methods
The sample comprised a total of 58 patients (35 f, 23 m) between the ages of 14 and 84 years (MW=58.61; SD=17.49). Of these, 11 patients were unilaterally deaf, of the 47 patients with bilateral deafness, 14 patients were fitted with CIs on both sides, 25 wore a hearing aid on the side not fitted with a CI, one wore a BAHA and 7 were unilaterally unaided. The measurements were taken at the beginning (T1) and end (T2) of the rehabilitation phase. The duration of the rehabilitation phase was quite different (M=6.8 months; SD=5.3 months), since every patient could spread the 30 appointments as time allowed. When those appointments were met and the patient was still in need of rehabilitation, another 15 appointments could be requested from the health insurance company of the patient. These appointment blocks of rehabilitation were called rehabilitation phases. Of the 58 patients, 34 were in their first rehabilitation phase, 24 were in the second or a later phase. The Freiburg mono- and multisyllabic speech test was administered one-sided under free-field conditions at 65 dB SPL with a one meter distance to the loudspeakers. The OLSA was administered under free-field condition: In quiet non-adaptive at 65 dB SPL, and in noise the L50 value was determined adaptively. Both the OLSA in quiet as well as in noise were tested in best-aided condition. The Freiburg mono- and multisyllabic test as well as OLSA in quiet were measured in percent of correctly repeated material, while the OLSA in noise was measured as L50 SNR. The comparisons between T1 and T2 were calculated using paired T-tests; Cohen’s d was used to calculate the effect sizes. The NCIQ results and the Freiburg and OLSA measurements were checked for correlations using Pearson’s correlations. All calculations were performed using SPSS25 (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.).
Results
Improvements in the NCIQ subscales, Freiburg speech test and OLSA
In all subcategories of the NCIQ, as well as in the total score, there were significant improvements within the measured rehabilitation phase. Effect sizes were small to medium, according to the recommendations of Cohen [8]. Patients who were measured in their first rehabilitation phase only showed significant increases in basic sound perception, self-esteem, activity limitation and social interaction. Only the patients in rehabilitation phase 2 or later also showed significant increases in advanced sound perception and speech production. There were also significant Improvements in the OLSA in noise and the Freiburg mono- and multisyllabic speech test, also with small to medium effect sizes [8]. Only OLSA in quiet showed no significant increase (see Table 1 [Tab. 1]).
Table 1: Results of paired T-tests (start/end of a rehabilitation phase) T2-T1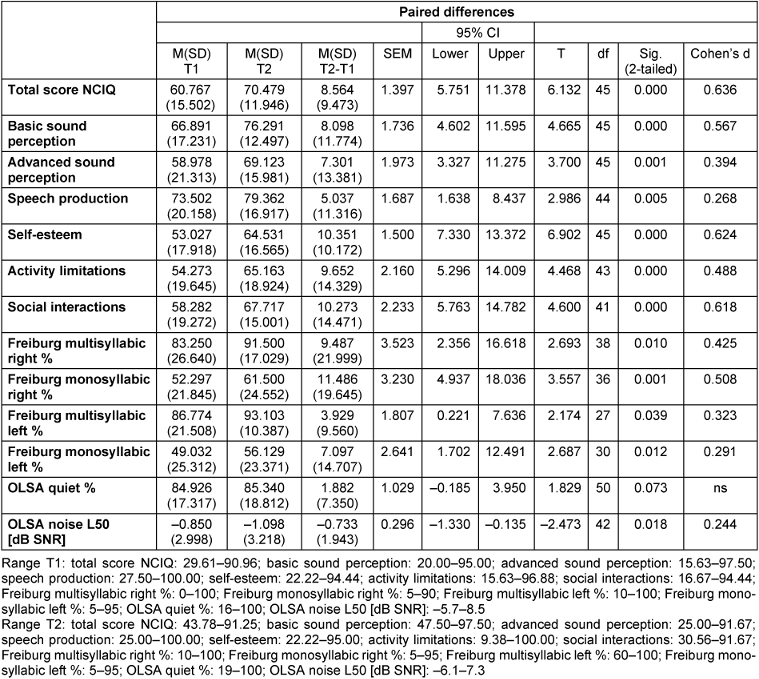
Correlations in NCIQ, OLSA and Freiburg speech test
At T1, the result of the OLSA in quiet, as well as the OLSA in noise, showed a significant correlation with basic sound perception, advanced sound perception and speech production of the NCIQ as measured at T1. The same variables showed significant correlations with the OLSA in noise at T2. However, regarding the OLSA in quiet, at T2 all subscales of the NCIQ showed significantly positive correlations (see Table 2 [Tab. 2]).
Table 2: Correlations OLSA (T1/T2) and NCIQ (T1/T2)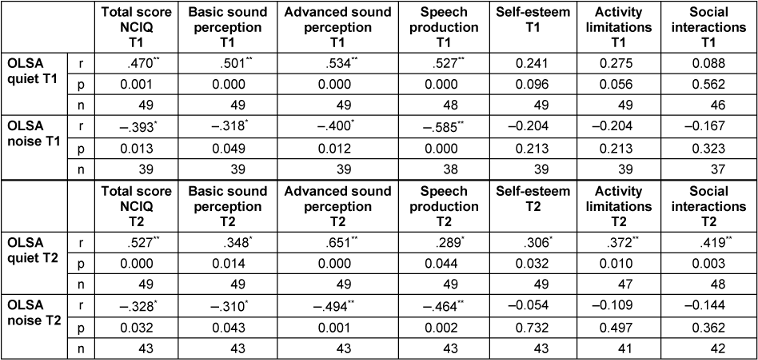
There were no significant correlations between the Freiburg mono- or multisyllabic speech tests and the NCIQ subscales, neither at T1, nor at T2.
Initial measurement and gain
In order to compare the initial measurements with the gain within a rehabilitation phase, the difference (delta) between T1 and T2 was calculated for each variable. The result was correlated with the measurement at T1. All correlations showed to be negative and significant at a p<.05 level (see Table 3 [Tab. 3]). Therefore, it could be shown that across all subcategories of the NCIQ, as well as in all audiological tests, the lower the initial value were, the higher the increases were within a rehabilitation phase.
Table 3: Correlations measurement T1 with gain between T1 and T2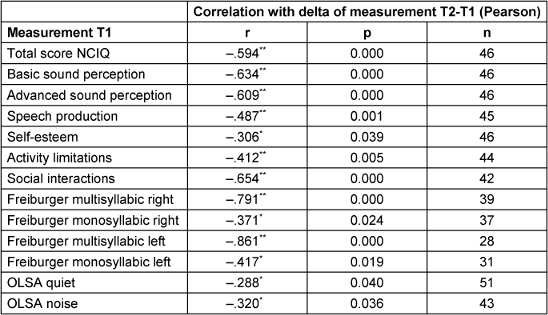
Gain in NCIQ, age and duration
The deltas between T1 and T2 regarding the subscales of the NCIQ were also correlated with the duration of the rehabilitation phase, as well as the age of the patients. It was shown that the older patients showed a higher increase in basic sound perception (r=.44; p=.003), advanced sound perception (r=.38; p=.011) and self-esteem (r=.347; p=.021). Also, age correlated negatively with the duration of the rehabilitation phase (r=–.300; p=.026). However, the duration of the rehabilitation phase showed no significant relationship with the gain in the subscales of the NCIQ.
Conclusion
Both the hearing measurement data and the NCIQ results show significant improvements within one rehabilitation phase. Significant increases in satisfaction with more complex listening tasks as well as increases in speech production only occur in later rehabilitation phases. However, all these are average values. In therapeutic contexts, it is always important to focus the individual, which may not show increases or even decreasing measures, especially in a subjective questionnaire which anchors on typical situations in everyday life. It is advisable to talk to the patient about such situations if the values, especially in the psychosocial subscales, deteriorate.
The correlations of the OLSA in quiet and in noise at T1 with the sound perception and speech production scales of the NCIQ suggest that the patients also subjectively rate their measured hearing ability as similarly high. At T2, the psychosocial subscales of the NCIQ also correlate with the result of the OLSA in quiet. It seems that, parallel to the objectively measured hearing gain in the course of the therapy, the patients also gain trust in their own ability to use their better hearing in everyday situations.
Patients with a poorer starting position seem to benefit the most across all tests. Longitudinal measures across the entire course of the therapy would be desirable to determine how the development continues and whether these are already signs of an early ceiling effect.
Older patients also showed more gains within a rehabilitation phase than younger patients, not only in sound perception, but also in their self-esteem, as measured by the NCIQ. This could point to a greater lack of possibilities for encouraging communicative situations in everyday life.
Notes
Conference presentation
This contribution was presented at the 26th Annual Conference of the German Society of Audiology and published as an abstract [9].
Competing interests
The authors declare that they have no competing interests.
References
[1] Andries E, Gilles A, Topsakal V, Vanderveken OM, Van de Heyning P, Van Rompaey V, Mertens G. Systematic Review of Quality of Life Assessments after Cochlear Implantation in Older Adults. Audiol Neurootol. 2021;26(2):61-75. DOI: 10.1159/000508433[2] Moberly AC, Harris MS, Boyce L, Vasil K, Wucinich T, Pisoni DB, Baxter J, Ray C, Shafiro V. Relating quality of life to outcomes and predictors in adult cochlear implant users: Are we measuring the right things? Laryngoscope. 2018 Apr;128(4):959-66. DOI: 10.1002/lary.26791
[3] McRackan TR, Bauschard M, Hatch JL, Franko-Tobin E, Droghini HR, Velozo CA, Nguyen SA, Dubno JR. Meta-analysis of Cochlear Implantation Outcomes Evaluated With General Health-related Patient-reported Outcome Measures. Otol Neurotol. 2018 Jan;39(1):29-36. DOI: 10.1097/MAO.0000000000001620
[4] Klop WM, Boermans PP, Ferrier MB, van den Hout WB, Stiggelbout AM, Frijns JH. Clinical relevance of quality of life outcome in cochlear implantation in postlingually deafened adults. Otol Neurotol. 2008 Aug;29(5):615-21. DOI: 10.1097/MAO.0b013e318172cfac
[5] Hirschfelder A, Gräbel S, Olze H. The impact of cochlear implantation on quality of life: the role of audiologic performance and variables. Otolaryngol Head Neck Surg. 2008 Mar;138(3):357-62. DOI: 10.1016/j.otohns.2007.10.019
[6] Hinderink JB, Krabbe PF, Van Den Broek P. Development and application of a health-related quality-of-life instrument for adults with cochlear implants: the Nijmegen cochlear implant questionnaire. Otolaryngol Head Neck Surg. 2000 Dec;123(6):756-65. DOI: 10.1067/mhn.2000.108203
[7] Deutsche Gesellschaft für Hals-Nasen-Ohren-Heilkunde, Kopf- und Hals-Chirurgie e.V. (DGHNO-KHC). S2K-Leitlinie Cochlea-Implantat-Versorgung. Register-Nr. 017/071. AWMF; 2020. Available from: https://www.awmf.org/uploads/tx_szleitlinien/017-071l_S2k_Cochlea-Implantat-Versorgung-zentral-auditorische-Implantate_2020-12.pdf
[8] Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Lawrence Erlbaum Associates; 1988.
[9] Metzeld D. Die Entwicklung der Lebensqualität und des Hörvermögens erwachsener CI-Träger im Verlauf der ambulanten CI-Folgetherapie. In: Deutsche Gesellschaft für Audiologie e.V., editor. 26. Jahrestagung der Deutschen Gesellschaft für Audiologie. Aalen, 06.-08.03.2024. Düsseldorf: German Medical Science GMS Publishing House; 2024. Doc021. DOI: 10.3205/24dga021




